Pulmonary hypertension isn't just high blood pressure in the lungs-it's a silent thief that slowly steals your ability to breathe, move, and live without exhaustion. It doesn't announce itself with a loud crash. Instead, it creeps in: a shortness of breath during your morning walk, fatigue that lingers after climbing stairs, swelling in your ankles that you blame on standing too long. By the time most people get diagnosed, the right side of their heart has already been working overtime for years. This isn't rare. About 1 in 100 people worldwide have it, and women are twice as likely to be affected. The good news? We know far more now than we did 20 years ago. With the right diagnosis and treatment, many people live much longer-and better-than they ever thought possible.
What Exactly Is Pulmonary Hypertension?
Pulmonary hypertension (PH) means the blood pressure in the arteries that carry blood from your heart to your lungs is too high. Normal pressure in these vessels is around 8-20 mmHg. When it climbs above 20 mmHg at rest-measured by the gold standard test called right heart catheterization-you’re looking at PH. This isn’t just a number. It’s a sign that the right ventricle, the chamber that pumps blood to the lungs, is struggling. Every beat becomes harder. The muscle thickens. The chamber stretches. And if left unchecked, it fails.
PH isn’t one disease. It’s five different groups, each with different causes:
- Group 1: Pulmonary arterial hypertension (PAH)-the rarest form, often with no clear cause, but sometimes linked to genetics or connective tissue diseases.
- Group 2: PH due to left heart disease, like heart failure or valve problems. This is the most common type.
- Group 3: PH caused by lung diseases such as COPD or pulmonary fibrosis.
- Group 4: Chronic thromboembolic PH (CTEPH)-caused by old blood clots that never dissolved and now block lung arteries.
- Group 5: PH with unclear or mixed causes, like kidney disease or blood disorders.
Knowing which group you’re in changes everything. Treatment for Group 1 is very different from Group 2 or 4. That’s why accurate diagnosis isn’t optional-it’s life-saving.
How Right Heart Strain Shows Up-Beyond the Symptoms
Most people with PH don’t feel pain. They feel tired. Breathless. Like they’re always one step behind their old self. But the real damage is happening inside the heart. Right heart strain shows up in measurable ways:
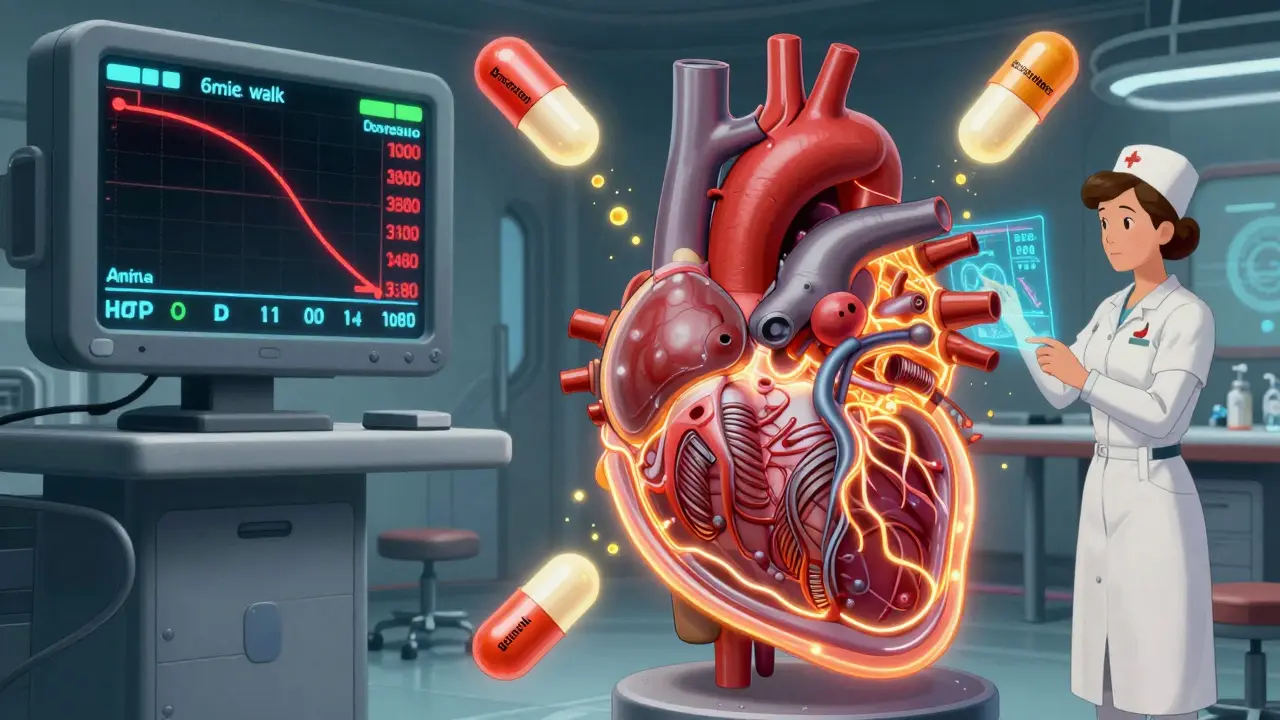
- Right ventricular hypertrophy: The wall of the right ventricle thickens beyond 5 mm on echocardiogram. It’s like your heart is lifting weights all day, every day.
- Right ventricular dilation: The chamber expands beyond 22 cm². It’s stretching too far, too fast, and losing its ability to pump efficiently.
- TAPSE less than 17 mm: This measures how much the tricuspid valve moves during a heartbeat. If it’s below 17 mm, the right ventricle is weak. This single number predicts survival better than many complex tests.
These aren’t just numbers on a screen. They’re signals your body is running out of reserves. A 6-minute walk test that gets you less than 380 meters? That’s a red flag. Studies show people who walk less than that are more than twice as likely to die within a year. BNP levels above 180 pg/mL or NT-proBNP over 1,400 pg/mL? Those biomarkers tell doctors your heart is under extreme stress. When these numbers rise, it’s time to act.
Many patients are misdiagnosed for years. One Reddit user shared: "My doctor said I was just out of shape for 18 months while my 6MWD dropped to 220 meters." That’s not uncommon. PH mimics asthma, COPD, anxiety-even aging. That’s why specialists look for the mismatch: someone with mild lung function but severe breathlessness. That’s PH.
Diagnosis: What Tests Really Matter?
Echocardiography is your first stop. It’s non-invasive, quick, and gives clues-like estimating pulmonary pressure, checking for right heart enlargement, and measuring TAPSE. But here’s the catch: echocardiograms overestimate pressure by 10-15 mmHg in nearly half the cases. They’re great for screening, but they can’t confirm PH.
Only one test gives the full picture: right heart catheterization. This is where a thin tube is threaded from your groin or neck into your heart to directly measure pressure in the pulmonary arteries. It’s the only way to know for sure if your pressure is above 20 mmHg. It also tells you whether the problem is in the lungs (pre-capillary) or the heart (post-capillary)-a critical difference.
Some people fear the procedure. It’s true: there are risks. About 3.4% of patients get an arrhythmia. 5.7% develop a hematoma. But for people with suspected PH, the risk of not doing it is far greater. As Dr. Nazzareno Galiè says: "Non-invasive methods cannot replace direct pressure measurement."
Cardiac MRI gives the most detailed view of the right ventricle-showing volume, function, and scarring. But it’s only available in 37% of specialized centers. That’s why echocardiography remains the workhorse, and catheterization remains the final answer.
Modern Therapy: From One Drug to Triple Therapy
Twenty years ago, the only option for PAH was oxygen and supportive care. Median survival? 2.8 years. Today? Five-year survival is over 60%. That’s because treatment has changed completely.
Now, most patients with Group 1 PAH start on combination therapy-two or even three drugs from different classes-right from diagnosis. This isn’t experimental. It’s standard. The REVEAL Registry shows 68% of PAH patients are on combination therapy as first-line treatment.
Here are the main drug classes:
- Endothelin receptor antagonists (ERAs): Bosentan, macitentan. Block chemicals that narrow blood vessels.
- Phosphodiesterase-5 inhibitors (PDE-5i): Sildenafil, tadalafil. Help relax lung arteries.
- Prostacyclin analogs: Epoprostenol (IV), treprostinil (inhalation or subcutaneous). Dilate vessels and prevent clots.
- Soluble guanylate cyclase stimulators: Riociguat. Boosts a natural pathway to relax arteries.
- Newcomer: Sotatercept: Approved in 2021, this is the first drug that doesn’t just treat symptoms-it targets the underlying cell growth causing vessel narrowing. In the STELLAR trial, it cut the risk of death or worsening by 44%.
For Group 4 (CTEPH), surgery to remove old clots (pulmonary thromboendarterectomy) can be curative. For others, anticoagulants and vasodilators help. But no one-size-fits-all approach works. That’s why treatment is personalized-based on symptoms, test results, and risk scores like REVEAL 2.0.
The Hidden Barriers: Delays, Costs, and Disparities
Even with better treatments, many people never get them. The average delay from symptom onset to diagnosis? 2.8 years. Nearly 8 out of 10 people are misdiagnosed first. In underserved communities, delays are 47% longer. Mortality rates are 32% higher.
Insurance is another wall. One survey found 63% of patients faced delays longer than 30 days for approval of IV prostacyclin therapies. These drugs cost tens of thousands per month. Without them, survival drops sharply. A PH nurse coordinator can cut hospitalizations by 27%-but many clinics don’t have one.
Specialized PH centers are rare. In the U.S., only 35 exist, yet they treat 75% of patients. If you’re not near one, you’re at a disadvantage. That’s why education for primary care doctors is now a top priority. Red flag symptoms? Progressive shortness of breath that doesn’t match lung function, unexplained right heart strain on EKG, and swelling without heart failure. If you see those, refer-don’t wait.
What Comes Next?
The future of PH care is here. Trials are testing let-7 microRNA as an early warning sign of right heart damage. Researchers are exploring drugs like dichloroacetate to fix the energy crisis in the right ventricle-because in PH, the heart doesn’t just pump harder, it runs out of fuel.
But the biggest breakthrough won’t come from a lab. It’ll come from faster diagnosis. From better training for doctors who see you first. From making sure no one waits two years to hear the word "pulmonary hypertension." Because when you catch it early, when you treat it aggressively, and when you support it with a team-survival isn’t just possible. It’s expected.