Over 80% of multiple myeloma bone disease patients suffer from severe bone damage, turning everyday movements into potential fractures. This condition is not just a side effect-it’s a core part of the disease driving pain, disability, and hospitalizations. Pathological fractures occur in 28-38% of patients, spinal cord compression in 5-10%, and hypercalcemia in 25-30%, making bone issues responsible for about 70% of myeloma-related suffering.
Understanding Multiple Myeloma Bone Disease
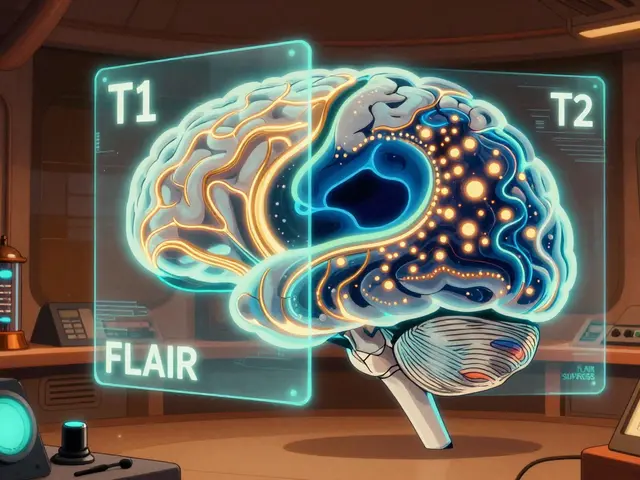
When doctors talk about multiple myeloma bone disease, they’re referring to the destructive changes in bones caused by cancerous plasma cells. Unlike normal bone loss from osteoporosis, myeloma bone disease creates "punched-out" holes visible on X-rays. These lesions form because myeloma cells disrupt the natural balance between bone building and breakdown. Healthy bones constantly remodel-old bone is removed by osteoclasts and new bone is built by osteoblasts. In myeloma, this process goes haywire. Osteoclasts become overactive while osteoblasts are suppressed, leading to rapid bone destruction without repair. This isn’t just a passive effect; bone damage actively fuels tumor growth through a vicious cycle. When bone is destroyed, it releases growth factors that feed myeloma cells, which then produce more factors that destroy more bone-a self-perpetuating loop.
The Science Behind Bone Destruction
The key player in this destruction is the RANKL pathway. Myeloma cells produce proteins that boost RANKL (Receptor Activator of Nuclear Factor Kappa-B Ligand) while reducing OPG (Osteoprotegerin), creating a 3-5 times higher RANKL/OPG ratio than healthy bones. This imbalance triggers excessive osteoclast activity. Another major factor is DKK1 (Dickkopf-1), a protein secreted by myeloma cells that blocks bone formation. Patients with DKK1 levels above 48.3 pmol/L have 3.2 times more bone lesions than those with lower levels. Sclerostin, a protein that inhibits bone building, is also elevated in myeloma patients (averaging 28.7 pmol/L vs 19.3 pmol/L in healthy individuals). Together, these mechanisms create a perfect storm where bone destruction outpaces repair.

Current Treatments: What Works and Where They Fall Short
Standard care for multiple myeloma bone disease includes intravenous bisphosphonates like Zoledronic acid or pamidronate, and the RANKL inhibitor Denosumab. Zoledronic acid (4mg monthly) reduces skeletal-related events by 15-18% compared to placebo, but 22% of patients need kidney dose adjustments due to renal toxicity. Denosumab (120mg monthly) offers similar protection with fewer kidney issues, though it carries a higher risk of osteonecrosis of the jaw (MRONJ). Despite these options, real-world data shows 68% of patients still experience persistent bone pain, and 42% develop MRONJ requiring dental procedures. Cost is another barrier-denosumab costs $1,800 per dose versus $150 for generic zoledronic acid, making it inaccessible for many outside the U.S.
| Treatment | Administration | Key Benefits | Limitations |
|---|---|---|---|
| Zoledronic acid | IV monthly | Cost-effective ($150 per dose) | 22% need renal dose adjustments |
| Denosumab | SC monthly | 74% patient preference for convenience | $1,800 per dose, MRONJ risk |
| Romosozumab (trials) | Subcutaneous | 53% BMD increase at spine | 12.3% hypocalcemia risk |
Breaking New Ground: Emerging Drugs in Clinical Trials
New therapies targeting specific pathways show real promise. Romosozumab, an anti-sclerostin antibody, increased bone mineral density by 53% at the lumbar spine in a 2021 trial with 49 myeloma patients. DKN-01, an anti-DKK1 therapy, reduced bone resorption markers by 38% in a phase Ib/II trial. Gamma-secretase inhibitors like nirogacestat cut osteolytic lesions by 62% in preclinical models. However, challenges remain-odanacatib (a cathepsin K inhibitor) was discontinued due to stroke risks, and most novel agents are still in early trials. The upcoming BONE-HEAL trial (NCT05218913) will test romosozumab in 450 patients over three years, aiming to confirm these early results. Researchers are also exploring bispecific antibodies that simultaneously target myeloma cells and bone microenvironment factors, with seven candidates now in phase I/II trials.

Real Patient Challenges: Pain, Costs, and Complications
Patient experiences highlight the human cost of bone disease. On the Myeloma Crowd Reddit community, a February 2023 thread with 147 comments revealed 68% still struggle with bone pain despite treatment. The International Myeloma Foundation’s 2022 survey of 1,247 patients found bone complications caused 32.7% of hospitalizations-second only to infections. Many report kidney issues from bisphosphonates (27% of zoledronic acid users) or MRONJ (42% of denosumab users). Cost barriers are stark: while 74% of patients prefer denosumab’s subcutaneous injection over IV therapy, the $1,800 price tag leaves many without access. "I had to choose between paying for my bone drug or my rent," shared one patient in a 2022 support group discussion. Renal toxicity from bisphosphonates requires frequent monitoring, with 22% of patients needing dose adjustments due to creatinine clearance below 60 mL/min. Dental evaluations within 30 days of starting therapy are critical to prevent MRONJ, but only 58% of patients receive this precaution.
The Future: Healing Bones, Not Just Slowing Damage
Researchers are moving beyond simply preventing bone loss to actively repairing damage. RNA therapies like ALN-DKK1 (from Alnylam) have reduced DKK1 by 65% in preclinical studies. The International Myeloma Foundation’s Dr. Brian Durie predicts: "By 2030, we will have moved from merely preventing bone destruction to actively healing myeloma bone lesions." This shift is critical-current treatments reduce skeletal-related events but don’t reverse existing damage. With new agents that stimulate bone formation, patients may soon avoid fractures and spinal cord compression altogether. The European Hematology Association’s 2023 guidelines now emphasize early intervention before skeletal-related events occur, shifting focus from reactive to proactive care. Global market projections show novel bone-targeting agents growing from $0.28 billion in 2022 to $1.5 billion by 2028, reflecting increasing investment in this space.
What causes bone damage in multiple myeloma?
Bone damage in multiple myeloma happens because cancerous plasma cells disrupt the normal bone remodeling process. They overactivate osteoclasts (bone-eating cells) through the RANKL pathway and suppress osteoblasts (bone-building cells) by secreting factors like DKK1 and sclerostin. This leads to "punched-out" lesions on X-rays and increases fracture risk.
How do current treatments for bone disease work?
Bisphosphonates like zoledronic acid bind to bone surfaces and slow osteoclast activity, reducing bone breakdown. Denosumab blocks RANKL, preventing osteoclast activation. These treatments reduce skeletal-related events by 15-18% but don’t rebuild bone. New agents like romosozumab target sclerostin to stimulate bone formation, showing promise in early trials.
What are the side effects of bisphosphonates?
Common side effects include kidney issues (22% of patients require dose adjustments), acute phase reactions (31.2%), and hypocalcemia. Long-term use increases the risk of osteonecrosis of the jaw (MRONJ), though this is less common than with denosumab. Regular kidney function tests are required during treatment.
Are there new drugs being developed for myeloma bone disease?
Yes, several promising agents are in trials. Romosozumab (anti-sclerostin) increased bone density by 53% in a phase II trial. DKN-01 (anti-DKK1) reduced bone resorption markers by 38%. Gamma-secretase inhibitors like nirogacestat cut lesions by 62% in preclinical studies. The BONE-HEAL trial is testing romosozumab in 450 patients for long-term effects.
What can patients do to protect their bones?
Patients should get a baseline skeletal survey and regular bone density scans. Calcium and vitamin D supplements are essential, especially with denosumab. Avoid high-impact activities that could cause fractures. Dental checkups before starting bone-targeting therapy reduce MRONJ risk. Work with a myeloma specialist to tailor treatment based on your bone health status.