
Drug Interaction Checker
Check Your Medication Combination
Enter the active ingredients in your medications to check for dangerous interactions.
Every winter, millions of people grab a bottle of cold medicine without reading the label. They think they’re doing the right thing-trying to feel better fast. But mixing allergy and cold meds can land you in the hospital. You might not even realize you’re taking the same active ingredient twice. And that’s just the start.
Why Combination Medications Are Risky
Most cold and allergy medicines you buy off the shelf aren’t just one drug. They’re cocktails. One pill might contain acetaminophen for fever, phenylephrine to unclog your nose, dextromethorphan to quiet your cough, and chlorpheniramine to stop your eyes from watering. It sounds convenient. But convenience kills when you don’t know what you’re swallowing.The FDA says these combination products make up 65% of all cold and allergy sales in the U.S. But they’re also responsible for 23% more side effects than single-ingredient options. Why? Because you’re stacking chemicals. And some of them don’t play nice together.
Take acetaminophen. It’s in more than 600 OTC products-from Tylenol to DayQuil to store-brand cold syrups. The safe daily limit is 4,000 mg. But if you take one tablet of Tylenol Sinus (500 mg acetaminophen) and then a spoonful of NyQuil (650 mg), you’re already over half your daily limit. Add a third product? You’re at risk of liver failure. The CDC estimates 6.7 million Americans accidentally overdose on acetaminophen every year-mostly from combining meds.
The Hidden Danger: Phenylephrine and Blood Pressure
You’ve seen it on the label: phenylephrine. It’s the decongestant in Sudafed PE, Mucinex D, and a hundred other brands. Manufacturers claim it shrinks swollen nasal passages. But here’s the truth: research from the University of Florida and Rutgers shows that 10 mg of oral phenylephrine does nothing better than a sugar pill. It doesn’t work as a decongestant at standard doses.And yet, it’s still everywhere. Why? Because it’s legal. Unlike pseudoephedrine (which is kept behind the pharmacy counter due to its link to meth production), phenylephrine is easy to sell. But here’s the kicker: when you combine phenylephrine with acetaminophen, your body absorbs four times more of it. That spikes your blood pressure-fast.
A 2014 study in New Zealand found phenylephrine-acetaminophen combos cause 4.1 times more hypertension-related side effects than acetaminophen alone. Symptoms? Dizziness, headaches, chest tightness, even heart palpitations. One Reddit user wrote: “Took two different cold meds thinking they were different-ended up in ER with high blood pressure.” That’s not rare. Emergency departments see it all the time.
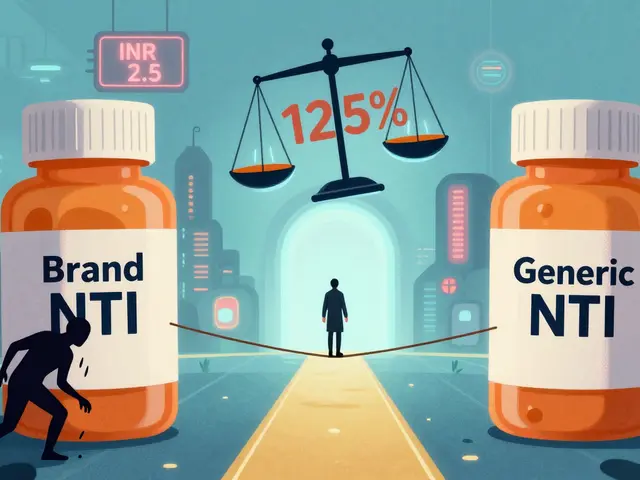
Pseudoephedrine: Stronger, But Riskier
If you want real decongestant power, you need pseudoephedrine. It’s in Sudafed, Claritin-D, and Zyrtec-D. Studies show it reduces nasal congestion by 65%, compared to just 45% with phenylephrine. But here’s the trade-off: pseudoephedrine raises your systolic blood pressure by 8-12 mmHg and your heart rate by 5-8 beats per minute. That’s not a small change.If you have high blood pressure-even if it’s just borderline-this can be dangerous. The FDA says avoid pseudoephedrine if your blood pressure is over 180/110. But most people don’t know their numbers. They just feel stuffed up and reach for the first bottle they see.
And if you’re on certain antidepressants? Forget it. Combining pseudoephedrine with MAOIs or tricyclics can cause sudden, life-threatening spikes in blood pressure. Desert Hope Treatment Center reports 15% of OTC-related ER visits involve cold meds mixed with antidepressants.
Dextromethorphan and the Serotonin Trap
Dextromethorphan (often labeled as “DM”) is the cough suppressant in Robitussin, Delsym, and many multi-symptom formulas. It’s generally safe when used alone. But when you mix it with SSRIs like sertraline (Zoloft), fluoxetine (Prozac), or SNRIs like venlafaxine (Effexor), you enter dangerous territory.Research from the Journal of Clinical Psychiatry in 2017 showed this combo increases serotonin syndrome risk by 300%. Serotonin syndrome isn’t just a headache. It’s a medical emergency: high fever, rapid heartbeat, confusion, muscle rigidity, seizures. It can kill.
Dr. Carter from SingleCare says: “People don’t realize their antidepressant and their cough syrup are fighting each other inside their body.” And because both are available over the counter, patients assume they’re safe together. They’re not.
How to Avoid a Dangerous Mix
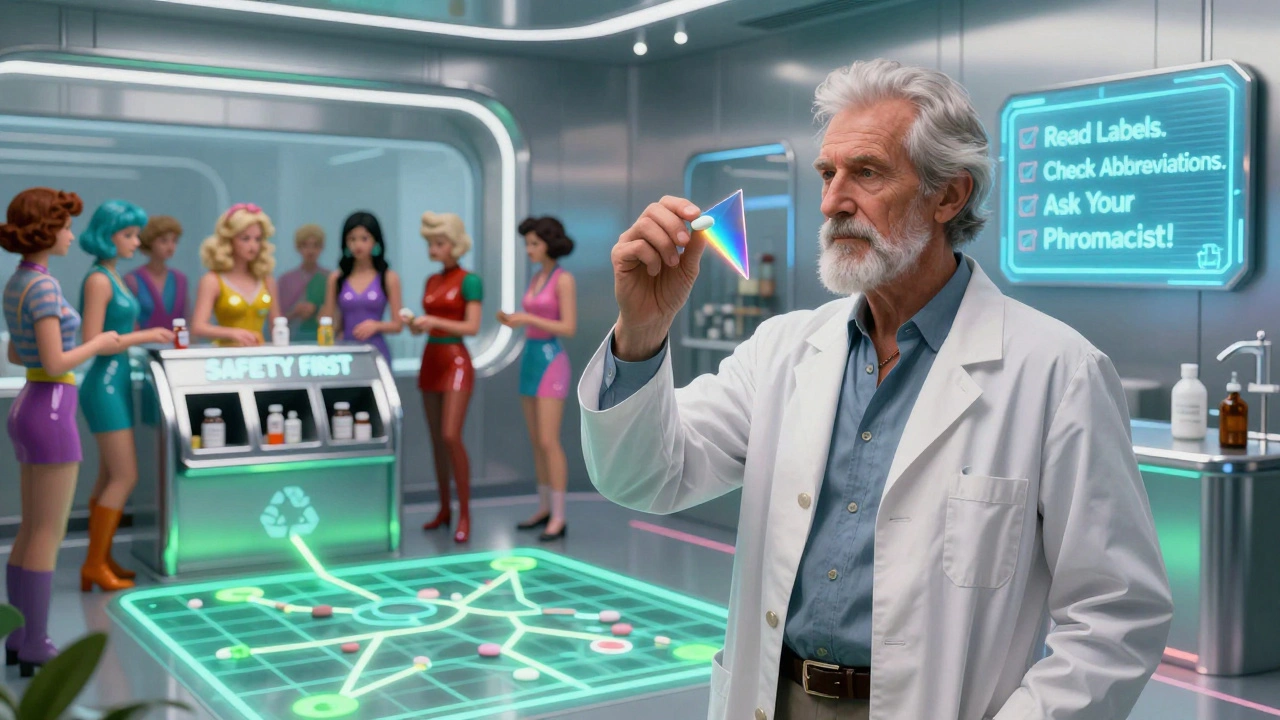
You don’t need to avoid cold meds entirely. You just need to be smarter. Here’s how:- Read the Drug Facts label-not just the brand name. Look for the “Active Ingredients” section. That’s where the real info lives.
- Know the abbreviations: APAP = acetaminophen, DM = dextromethorphan, PE = phenylephrine, PSE = pseudoephedrine, CL = chlorpheniramine, DP = diphenhydramine.
- Never take two products with the same active ingredient. If you’re already taking a cold medicine with acetaminophen, don’t also take Tylenol or Excedrin.
- Check with your doctor or pharmacist if you’re on prescription meds-especially for depression, anxiety, heart conditions, or high blood pressure.
- Use a drug interaction checker. Apps like Medisafe or WebMD’s tool scan your meds and warn you about clashes. They process over a million checks daily.
Most people spend less than 30 seconds picking a cold medicine. That’s not enough. The American Pharmacists Association recommends 15-20 minutes to review all your options. Take that time. It could save your liver, your heart, or your life.
What to Do If You’ve Already Mixed Them
If you took two cold meds and now feel dizzy, your heart is racing, or your stomach feels off-don’t wait. Call Poison Control at 1-800-222-1222 (U.S.) or go to your nearest ER. Don’t assume it’s “just a side effect.” Acetaminophen overdose can take 24-48 hours to show symptoms. By then, liver damage may already be irreversible.If you’re unsure what you took, bring the bottles with you. Pharmacists can decode the labels faster than you can. And if you’re on antidepressants or blood pressure meds, tell them upfront. That context changes everything.
What’s Changing in 2025?
The FDA is finally acting. By December 2024, all combination cold and allergy products must have high-contrast labels with bold warnings about duplicate ingredients. They’re also reviewing phenylephrine’s effectiveness. If the September 2023 advisory committee’s findings hold, many products may be pulled from shelves-or reformulated.Some manufacturers are already switching. McNeil (Tylenol’s maker) has filed patents for new formulas using caffeine and guaifenesin instead of phenylephrine. That could mean safer options soon. But until then, you’re on your own.
Single-Ingredient Is Safer
Here’s the hard truth: if you only have a runny nose, take an antihistamine. If you only have a cough, take dextromethorphan alone. If you only have a headache, take acetaminophen or ibuprofen by itself.Yes, it’s less convenient. But it’s safer. And it’s cheaper. Single-ingredient meds average 7.2 out of 10 in user ratings on Drugs.com. Combination products? Just 5.8. People don’t like the side effects. They don’t like the confusion. And they don’t like ending up in the ER.
Next time you’re reaching for a cold medicine, ask yourself: Do I really need all these ingredients? Or am I just being sold a solution that’s more dangerous than the problem?”
Can I take allergy medicine with a cold medicine?
Only if you check the active ingredients. Many allergy meds (like Claritin-D or Zyrtec-D) already contain decongestants. Adding a cold medicine with the same ingredient can lead to overdose. Always compare labels. If both have pseudoephedrine or phenylephrine, don’t combine them.
Is it safe to take Tylenol with a cold medicine?
Only if the cold medicine doesn’t already contain acetaminophen. Many cold and flu products include acetaminophen (listed as APAP). Taking extra Tylenol on top of that can cause liver damage. Always check the label. If you’re unsure, skip the extra pain reliever.
What happens if I mix cold medicine with antidepressants?
It can be life-threatening. Dextromethorphan (in cough syrups) combined with SSRIs or SNRIs can cause serotonin syndrome. Pseudoephedrine can spike blood pressure dangerously when mixed with MAOIs or tricyclics. Never combine these without talking to your doctor first.
Are phenylephrine cold medicines still safe to use?
They’re legal, but they’re not effective. Research shows 10 mg of oral phenylephrine doesn’t work better than a placebo as a decongestant. Worse, when paired with acetaminophen, it increases blood pressure risks. If you need a decongestant, pseudoephedrine works better-but only if you don’t have high blood pressure or heart issues.
How do I know if I’ve taken too much acetaminophen?
Early signs include nausea, vomiting, loss of appetite, and sweating. But liver damage may not show symptoms for days. If you’ve taken more than 4,000 mg in 24 hours-or you’re unsure-call Poison Control immediately. Don’t wait for symptoms. Acetaminophen overdose is treatable if caught early.
What’s the safest cold medicine to take?
The safest option is a single-ingredient medicine that matches your symptom. For a runny nose: an antihistamine like loratadine. For a cough: dextromethorphan alone. For a headache: plain acetaminophen or ibuprofen. Avoid multi-symptom formulas unless you have all the symptoms they treat-and you’ve confirmed no ingredient overlaps with your other meds.
Next Steps
- Write down every medication you take daily-including vitamins and supplements. - Bring that list to your next doctor or pharmacist visit. - Download a barcode-scanning app like Medisafe or MyTherapy. - When buying cold meds, ask the pharmacist: “Does this contain anything I’m already taking?” You don’t need to suffer through a cold. But you do need to be smart about how you treat it. One wrong mix can undo months of good health. Don’t gamble with your liver. Don’t risk your heart. Read the label. Twice.Shubham Mathur
People still buy those multi-symptom cold pills like they’re buying candy? Bro. You’re literally stacking chemicals like a drunk chemist. I took NyQuil and DayQuil back-to-back last winter-thought I was being smart. Woke up sweating, heart racing, felt like my skull was gonna explode. Turned out I hit 5,000mg of acetaminophen. ER visit. $1,200 bill. Never again. Read the damn label. APAP isn’t a brand-it’s a death sentence if you ignore it.
Stacy Tolbert
I cried reading this. My mom did this last year. She took Zyrtec-D and Robitussin because she ‘just wanted to sleep.’ Ended up in ICU with serotonin syndrome. She’s fine now but she won’t touch OTC meds without me checking them first. I keep a printed list of all her meds taped to the fridge. It’s sad we have to be our own pharmacists.
Ronald Ezamaru
Phenylephrine is a scam. Full stop. The FDA advisory committee called it ineffective in 2023 and yet it’s still in 80% of store-brand cold meds because it’s cheaper and easier to stock than pseudoephedrine. The real tragedy? People think they’re getting relief when they’re not. It’s placebo with side effects. If you need a decongestant, go behind the counter and ask for pseudoephedrine. Yes, you’ll need ID. Yes, they’ll limit the quantity. But at least you’ll get something that works. And if you’re hypertensive? Skip it. Your blood pressure doesn’t need another enemy.
Ryan Brady
Why are we even talking about this? It’s 2025. We have smartphones that can track our heart rate and sleep cycles but we still can’t read a medicine label? This is why America’s healthcare costs are insane. People are lazy. They want a pill for everything and don’t want to think. The real solution? Ban combination meds. Make everything single-ingredient. Make people work for it. If you can’t handle reading two lines of text, maybe you shouldn’t be medicating yourself.
Suzanne Johnston
There’s a deeper cultural issue here. We’ve been conditioned to believe that ‘more’ means ‘better.’ More ingredients = more healing. But biology doesn’t work that way. The body isn’t a machine you can upgrade with a multipack. It’s a fragile ecosystem. Every chemical you introduce is a ripple. We treat medicine like a buffet-grab what looks good-and forget we’re not just feeding our symptoms, we’re feeding our physiology. The real question isn’t ‘what’s in the bottle?’ It’s ‘why do we think we need so much?’
Graham Abbas
Let me tell you about my cousin in Manchester-he took a cold med with phenylephrine and his blood pressure spiked so hard he passed out on the bus. No history of hypertension. Just a guy trying to get through a cold. Now he’s on beta-blockers. He didn’t even know the medicine had decongestants in it. The label was printed in 6pt font on a white background. How is that acceptable? We need regulation that doesn’t assume everyone’s a pharmacist. This isn’t just about drugs-it’s about design. If it’s dangerous, it shouldn’t be hidden.
Haley P Law
OMG I JUST REALIZED I’VE BEEN DOING THIS FOR YEARS 😭 I take Zyrtec-D for allergies and then NyQuil for sleep? I thought they were different because one says ‘allergy’ and one says ‘cold’-but they both have pseudoephedrine and dextromethorphan?? I’m gonna throw out my entire medicine cabinet right now. My heart is pounding just thinking about it. Someone get me a therapist and a barcode scanner. 🥲🩺
Andrea DeWinter
One thing people don’t mention: pharmacies don’t always help. I asked a pharmacist about mixing my Zoloft with a cough syrup and she just said ‘probably fine.’ I left unsatisfied. So I used Medisafe. It flagged the interaction in 3 seconds. That’s the problem-we rely on people who are overworked and undertrained. Tech tools like Medisafe or WebMD’s checker aren’t just convenient-they’re lifesavers. Use them. Even if you think you know what you’re doing. You don’t. I didn’t.
George Taylor
Look. This post is 90% fearmongering. Yes, there are risks. But people have been mixing cold meds since the 1950s and we’re still here. The FDA doesn’t ban things because they’re risky-they ban them because they’re ineffective or *consistently* lethal. Phenylephrine doesn’t kill people. Bad labeling does. And yes, acetaminophen overdose is bad-but so is ignoring your symptoms and letting a cold turn into pneumonia. You’re not a lab rat. You’re a human. Use common sense. Don’t take 10 pills. Take one. Read the label. Done. This article reads like a public service ad written by a panic-prone med student.
Chris Marel
Back home in Nigeria, we don’t have these fancy combination pills. We buy one thing for fever, one for cough, one for runny nose. It’s cheaper and safer. People here in the US are so used to convenience that they forget medicine isn’t fast food. I showed my cousin here how to read labels. He said, ‘Why not just take one pill?’ I told him: because one pill might be five pills in disguise. He didn’t believe me until he checked his own bottle. Now he brings every new med to me before he takes it. Small acts save lives.
Arun Kumar Raut
Simple rule: if it has more than one thing in it, don’t take it unless you have all the symptoms. If you have a cough, take cough medicine only. If you have a runny nose, take allergy medicine only. No need for fever stuff if you’re not feverish. Don’t overcomplicate. Medicine is not a buffet. It’s a tool. Use one tool at a time. Easy.
precious amzy
One cannot help but observe the epistemological collapse implicit in the commodification of pharmaceutical self-care. The neoliberal imperative to optimize one’s corporeal state through instantaneous, market-driven pharmacological intervention has rendered the layperson not merely a consumer-but a unwitting pharmacokinetic agent in a system predicated on obfuscation and profit maximization. The FDA’s tepid regulatory response is symptomatic of a broader cultural malaise wherein scientific literacy is subordinated to brand recognition. One must ask: Is the danger not the drug, but the ideology that permits its proliferation?


Write a comment