
Why Sarcopenia in COPD Is More Than Just Weakness
When you have COPD, your lungs struggle to give you enough air. But what most people don’t realize is that your muscles are struggling too. About 1 in 5 people with COPD also have sarcopenia - a loss of muscle mass, strength, and function that isn’t just from getting older. It’s caused by a mix of low oxygen, inflammation, inactivity, and not eating enough protein. This isn’t just about feeling tired. It’s about whether you can stand up from a chair, walk to the bathroom, or carry your groceries. Without intervention, sarcopenia cuts your life expectancy by 20-40% compared to COPD patients who still have strong muscles.
How Sarcopenia in COPD Is Different From Normal Aging
Age-related muscle loss usually hits your legs first. In COPD, it hits your breathing muscles - your diaphragm, your chest - and your arms harder. Studies using CT scans show that 68% of COPD patients have visibly shrunken pectoral muscles, compared to just 22% of healthy older adults. Your muscles aren’t just getting smaller; they’re losing strength faster. While healthy people lose about 1-2% of muscle mass per year after 60, people with COPD lose up to 3.2% annually. And it’s not just physical inactivity. Low oxygen levels at night - common in advanced COPD - directly trigger muscle breakdown. If your oxygen drops below 88% for more than 30% of your sleep, your risk of severe sarcopenia jumps by nearly half.
How Doctors Diagnose Sarcopenia in COPD Patients
Screening isn’t optional anymore. The American Thoracic Society now recommends all COPD patients be checked for sarcopenia. The simplest test? Handgrip strength. If you’re a man and your grip is under 27 kg, or a woman under 16 kg, that’s a red flag. But grip alone isn’t enough. Doctors also use the Short Physical Performance Battery (SPPB), which measures how fast you walk 4 meters, how long you can stand on one foot, and how many times you can stand up from a chair in 30 seconds. A score of 8 or lower means you’re at risk. For more detail, imaging like CT scans at the L3 spine level can measure muscle area. In COPD patients, a muscle index below 55 cm²/m² for men and 39 cm²/m² for women confirms sarcopenia - thresholds lower than those used for healthy older adults because COPD changes body composition.
The Two Pillars of Treatment: Protein and Resistance Training
There’s no magic pill. The only proven way to fight sarcopenia in COPD is combining better nutrition with smart strength training. But the rules are different than for healthy people.
Nutrition: More Protein, Spread Out
Most COPD patients eat only 0.8-1.0 grams of protein per kilogram of body weight daily. The target? 1.2-1.5 grams per kg. That means a 70 kg person needs 84-105 grams of protein every day - not just at dinner. Spread it across 4 meals: 20-25 grams per meal. Why? Your muscles can only use so much protein at once. Eating it evenly boosts muscle building all day. Add 2.5-3 grams of leucine per meal - a key amino acid found in whey protein, eggs, chicken, and soy. Studies show this increases muscle protein synthesis by 37% in sarcopenic COPD patients. If eating enough is hard because of breathlessness or loss of appetite, whey protein shakes with 10g leucine can help. They’re easier to swallow, digest quickly, and don’t fill you up like a big meal.
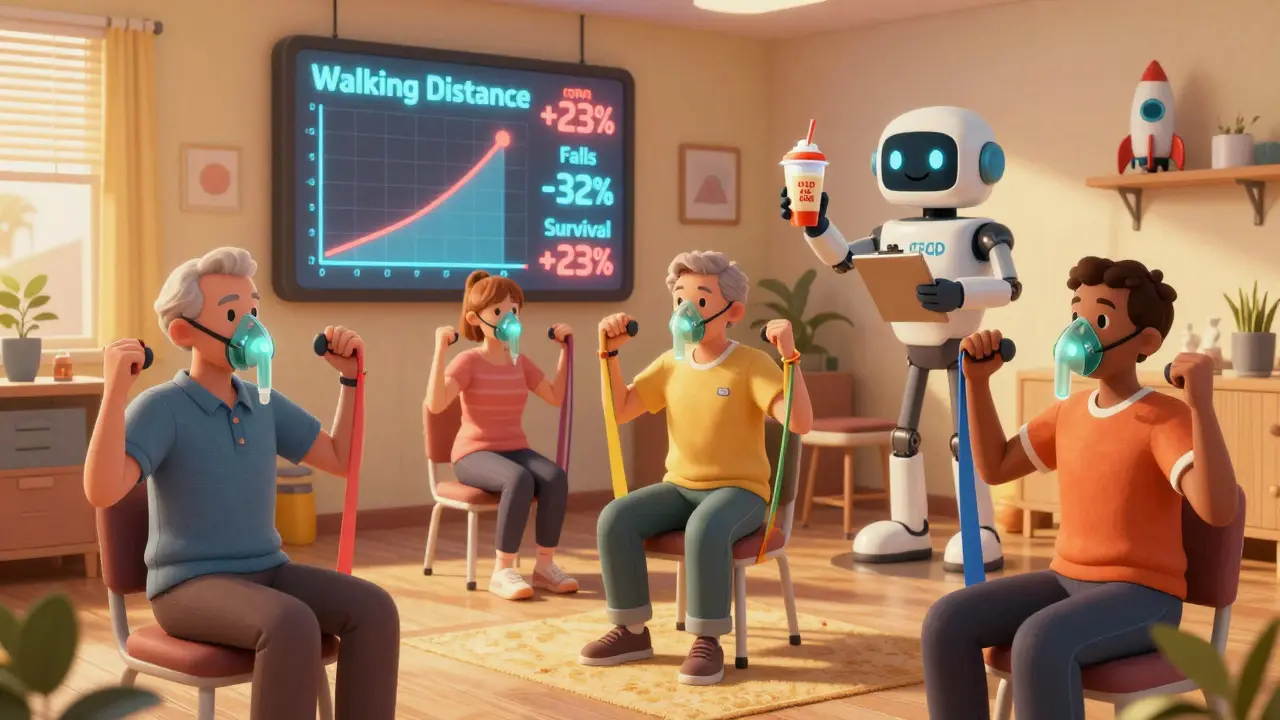
Resistance Training: Start Light, Go Slow
Traditional gym routines won’t work. Most COPD patients can’t handle heavy weights or short rest periods. The key is low intensity, high tolerance. Start with 30-40% of your one-rep max - that’s about 1-5 pounds for most people. Use resistance bands, light dumbbells, or even bodyweight exercises like seated marches or wall push-ups. Do 2-3 sessions a week, targeting arms, legs, and core. Rest 2-3 minutes between sets. If you’re short of breath, stop. Don’t push through it. Many patients need supplemental oxygen during training - up to 42% do. That’s not a failure; it’s part of the plan. Progress slowly. It takes 8-12 weeks to see real strength gains, but the payoff is huge: 23% improvement in walking distance, better balance, and fewer falls.
What Works - Real Patient Stories
Mary Thompson, 68, with GOLD Stage 3 COPD, started with resistance bands and a daily whey shake after her pulmonary rehab program. Within 12 weeks, she could carry her grocery bags without stopping. "I didn’t think I’d ever do that again," she said. John Peterson, 72, with Stage 4 COPD, tried resistance training without oxygen support and had to quit after three sessions. "I couldn’t breathe," he wrote. His story isn’t uncommon. But when training is adjusted - lower weight, longer rests, oxygen if needed - success rates jump. At the Cleveland Clinic, 78 patients with sarcopenia and COPD improved their 6-minute walk distance by 23% after 16 weeks of supervised training and protein supplements.
Why So Many People Fail - And How to Avoid It
Three big reasons people quit: dyspnea, poor protein intake, and giving up during flare-ups. Forty-two percent need oxygen during training. If your program doesn’t offer it, you’re set up to fail. Half of patients eat less than half the protein they need. And during a COPD flare-up, 57% stop exercising entirely. That’s dangerous. Muscle loss accelerates during exacerbations. The fix? Keep moving - even if it’s just seated arm curls or ankle pumps. And keep eating protein. A simple shake during a flare can help slow muscle breakdown. Don’t wait until you feel better to start again.
What’s Next: New Treatments on the Horizon
Research is moving fast. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) released its first sarcopenia management algorithm in early 2024, linking nighttime oxygen levels to exercise prescriptions. Early results show a 29% slowdown in muscle loss. A major European trial is testing HMB - a supplement that helps preserve muscle - combined with resistance training. And a new drug, PTI-501, a myostatin inhibitor, is in phase 2 trials specifically for COPD-related muscle loss, with results expected in mid-2025. These aren’t cures, but they’re promising tools. Right now, though, the best treatment is still nutrition and movement - done right.
Can You Reverse Sarcopenia in COPD?
Yes - but not overnight. You won’t regain the muscle you lost in your 40s or 50s. But you can stop the decline. You can get stronger. You can walk farther, climb stairs, stand up without help. Studies show that with consistent protein and resistance training, 5-year survival for severe COPD patients with sarcopenia jumps from 45% to 68%. Hospitalizations drop by 32%. Quality of life improves. It’s not about becoming an athlete. It’s about keeping your independence. And that’s worth every effort.
How do I know if I have sarcopenia with COPD?
Start with a handgrip strength test - under 27 kg for men or 16 kg for women is a warning sign. Your doctor may also check your walking speed, chair stands, and balance using the SPPB test. If you’re struggling with daily tasks like carrying groceries or standing from a chair, and you have COPD, ask for a screening. Imaging like a CT scan can confirm muscle loss if needed.
How much protein should I eat if I have COPD and sarcopenia?
Aim for 1.2 to 1.5 grams of protein per kilogram of body weight every day. For example, if you weigh 70 kg, that’s 84-105 grams daily. Split it into 4 meals - about 20-25 grams per meal - to help your muscles use it best. Include leucine-rich foods like eggs, chicken, fish, soy, or whey protein shakes. Many people need supplements because eating enough food is hard with breathlessness.
Can I do resistance training if I’m short of breath?
Yes - but you need to adjust. Start with very light weights or resistance bands. Do fewer reps, rest longer between sets (2-3 minutes), and use supplemental oxygen if your doctor recommends it. Don’t push through breathlessness. Stop and breathe. Many people need oxygen during training - it’s normal, not a failure. Work with a pulmonary rehab specialist who knows how to adapt exercises for COPD.
What if I can’t eat enough protein because I’m not hungry?
Try liquid nutrition. Whey protein shakes with 10g leucine are easy to drink, digest quickly, and don’t fill you up. Have one after waking up, after a short walk, and before bed. Eat smaller, more frequent meals. Add powdered protein to soups, mashed potatoes, or oatmeal. If appetite stays low, talk to your doctor about appetite stimulants or nutritional counseling - this is common in advanced COPD.
Does oxygen therapy help with muscle loss in COPD?
Yes - especially at night. Low oxygen during sleep directly causes muscle breakdown. If your oxygen drops below 88% for more than 30% of your sleep, nighttime oxygen therapy can slow sarcopenia. During exercise, supplemental oxygen also lets you train longer and harder without triggering severe breathlessness. Ask your doctor for a sleep study and an exercise oxygen test to see if you need it.
What to Do Next
Don’t wait for symptoms to get worse. If you have COPD and feel weaker, less able to do daily tasks, or have lost weight without trying, ask your doctor for a sarcopenia screening. Request a referral to pulmonary rehabilitation - it’s covered by most insurance. Start with protein: calculate your daily need and aim to hit it. Then, begin light resistance training - even seated exercises count. You don’t need a gym. You need consistency. And you need to keep going, even when it’s hard. The goal isn’t to run a marathon. It’s to carry your own laundry. To stand up without help. To live longer, and better.
James Hilton
So let me get this straight - we’re telling people with COPD to lift weights and chug protein shakes like they’re prepping for a bodybuilding contest? Bro, I’ve seen grandmas struggle to open jars. This isn’t fitness porn. It’s survival. And somehow, the docs still act like it’s a choice.
Mimi Bos
i just read this and thought of my dad… he’s 74 with copd and barely eats anything cause he gets too tired. i started slipping whey powder into his oatmeal and he actually said he feels a lil less wiped out. not magic, but… it’s somethin.
sonam gupta
western medicine always overcomplicates everything protein and movement been around for centuries why do we need ct scans and leucine supplements
oluwarotimi w alaka
this is what happens when you let the globalist medical cartel take over. they don’t want you strong - they want you dependent. protein? resistance training? nah. they’d rather you take their pills, sit in their oxygen tents, and pay for their "rehab" programs that cost more than your car. wake up. your muscles aren’t broken - your system is rigged.
Sydney Lee
The irony is palpable: we’ve reduced human resilience to a biomechanical algorithm - protein per kilogram, muscle index thresholds, SPPB scores - as if the soul of strength can be quantified by a spreadsheet. We have forgotten that movement is not therapy; it is rebellion. And yet, here we are, measuring dignity in centimeters squared.
Vu L
Wait so you’re telling me the real cure for COPD isn’t vaping or quitting smoking but… doing squats? I’m out. This is the dumbest thing I’ve read all week.
Celia McTighe
this made me cry a little 😭 my aunt did exactly this - started with seated arm circles and a protein shake every morning. she went from needing help to the bathroom to walking around the block. it wasn’t pretty, but it was hers. you don’t have to be strong to start. you just have to start.
Ryan Touhill
I find it fascinating how the medical establishment has co-opted the language of empowerment while maintaining structural control. Resistance training? Protein? These are not solutions - they are distractions from the real issue: systemic neglect of chronic illness in favor of profit-driven pharmaceutical interventions. The patient is not a problem to be optimized - they are a subject to be managed.
Julius Hader
i’ve been doing this for 8 months now. 20g protein at breakfast, light bands 3x a week. i can finally pick up my grandkid without wheezing. it’s not a miracle. it’s just… not giving up. 🙏
Debra Cagwin
To anyone feeling overwhelmed - start with one thing. One protein shake. One set of seated marches. One day. Progress isn’t linear, but it’s real. You’re not failing because you’re tired. You’re human. And humans, even with broken lungs, are capable of astonishing resilience. I believe in you.
Kelsey Youmans
The clinical data presented here is both compelling and methodologically rigorous. It is imperative that healthcare providers integrate these evidence-based protocols into standard pulmonary rehabilitation frameworks, particularly in underserved populations where access to nutritional counseling and supervised resistance training remains inadequate.
Hakim Bachiri
Let’s be real - this whole thing is just a capitalist scam. Protein shakes? $30 a tub. Resistance bands? $25. Oxygen during exercise? Insurance won’t cover it unless you’re dying. Meanwhile, the real answer is simple: stop breathing polluted air. But who’s gonna sue the factories? Nobody. So we just make people lift dumbbells while the world burns.
Payton Daily
You know what’s wild? The body doesn’t care about your diagnosis. It doesn’t know COPD from a Tuesday. It just knows: use it or lose it. And if you feed it protein, it’ll try. Not because it’s smart. Because it’s alive. And if you’re still breathing - even if it’s ragged, even if it hurts - your muscles are begging you to move. Not for a number. Not for a study. Just to feel like you still belong in your own skin.





Write a comment