Imagine this: you leave your doctor’s office with a new prescription, feeling hopeful. But at the pharmacy, the pharmacist says your copay is $350. You didn’t know. You didn’t ask. And now you’re stuck-either pay it, skip the medication, or go back to your doctor. This happens to 22% of people in the U.S. every year, according to GoodRx. Most of them never saw it coming. The fix? Talk about cost before you get the script.
Why Cost Talks Before Prescribing Matter
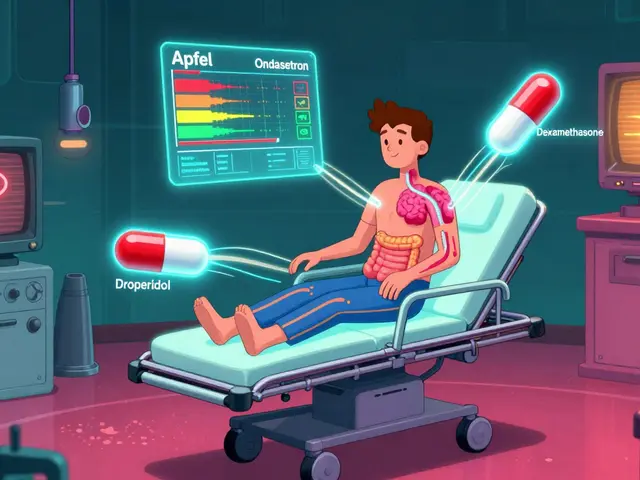
It’s not just about saving money. It’s about sticking to your treatment. A 2022 study in the Journal of General Internal Medicine found that patients who talk about cost with their doctor are 37% less likely to skip doses or stop taking their meds because of price. That’s huge. Skipping insulin, blood pressure pills, or antidepressants doesn’t just hurt your health-it leads to ER visits, hospital stays, and higher long-term costs. The system is changing. Thanks to the Inflation Reduction Act of 2022, Medicare Part D now has a hard cap on out-of-pocket drug spending: $2,100 in 2026. That’s down from $8,000 in 2024. And insulin? No more than $35 a month. But these rules only apply if you know to ask. And if you’re on a commercial plan, you’re still on your own-most don’t have an annual cap.Know Your Insurance Before You Walk In
Your insurance plan has something called a formulary. That’s just a fancy word for the list of drugs they cover-and how much you pay for each. Most plans split drugs into tiers:- Tier 1 (Generic): $5-$15 copay
- Tier 2 (Preferred Brand): $25-$50
- Tier 3 (Non-Preferred Brand): $50-$100
- Specialty Tier: 25-33% coinsurance, sometimes $100+ per fill
Ask These Five Questions at Your Appointment
Don’t wait for your doctor to bring it up. Bring it up yourself. Here’s what to say:- “Is there a generic version of this drug?” Generics work the same but cost 80% less on average.
- “What’s my out-of-pocket cost with my insurance?” Don’t accept “I don’t know.” Ask them to check your plan’s formulary.
- “Are there other medications that treat the same thing but cost less?” Sometimes a different brand or class of drug works just as well.
- “Can I get this through mail order?” Many plans offer 90-day supplies at lower prices. Some even ship free.
- “Is there a patient assistance program?” Drugmakers like Pfizer, Merck, and Novo Nordisk offer discounts or free meds to low-income patients. Your pharmacist can help you apply.
Use Tools That Actually Save Money
There are apps and websites built just to help you compare prices. GoodRx is the most popular. It shows you cash prices at pharmacies near you-even if you have insurance. Sometimes, paying cash with a GoodRx coupon is cheaper than using your insurance. One user in Perth saved $287 on blood pressure meds this way. Other tools like SingleCare and RxSaver work similarly. Enter your drug, zip code, and see the lowest price within 5 miles. Some pharmacies even let you text your prescription number to get a quote before you walk in. If you’re on Medicare, don’t forget the Medicare Prescription Payment Plan. Starting in 2025, you can spread your drug costs over 12 months. Pay $175 a month instead of $2,100 all at once. But here’s the catch: you have to sign up before September. If you wait until November, you won’t get the full benefit.Timing Is Everything
If you’re on a high-deductible plan, January through March is the worst time to fill prescriptions. You haven’t met your deductible yet, so you pay full price. A 2023 KFF analysis found that individual marketplace plans averaged a $480 deductible. That means if your drug costs $200, you pay $200-until you hit that $480 mark. Plan ahead. If you know you’ll need a new prescription in February, ask your doctor to write it in December. Fill it in January so it counts toward your deductible. Or ask for a 3-month supply upfront. Some insurers let you do that without extra cost.
What If Your Drug Isn’t Covered?
About 43% of prescription cost problems come from drugs not being on your plan’s formulary. That doesn’t mean you’re out of luck. Your doctor can file a prior authorization request. That’s just a formal appeal asking your insurer to cover the drug anyway. Most of the time, it works-if you have a good reason. Examples: “This drug controls my seizures better than the alternatives.” or “I had a bad reaction to the covered version.” Your doctor’s office handles the paperwork. You just need to ask them to do it. If the appeal gets denied, ask your pharmacist about therapeutic alternatives. Sometimes, a different drug in the same class is covered. Or ask your doctor to switch you to a different treatment plan entirely.Real Stories, Real Savings
One Reddit user, “MedicareMom2023,” avoided a $1,200 monthly bill by checking her plan’s formulary before her appointment. She found a cheaper alternative her doctor didn’t know about. Another person, who got a new diabetes script, walked into the pharmacy expecting $30-and was hit with $350. They abandoned the med. 87% of commenters on that post said they’d done the same. The difference? One person asked questions. The other didn’t.What to Do Right Now
You don’t need to wait for your next appointment. Here’s your action plan:- Log into your insurance website. Search your current meds. Write down the copay for each.
- Download GoodRx. Search your top 3 prescriptions. Compare cash price vs. insurance price.
- Next time you see your doctor, say: “Can we check if this new prescription is covered and what it’ll cost?”
- If you’re on Medicare, go to Medicare.gov and use the Plan Finder. Even if you’re happy with your plan, it pays to check.
- Keep a note on your phone: “Drugs I take + their cost.” Update it every time you refill.
What if my insurance says a drug is covered but the pharmacy says it’s not?
This happens when your plan’s formulary changes after your doctor writes the script. Call your insurer with the drug’s NDC number (found on the bottle) and ask for a real-time cost check. If they say it’s covered but the pharmacy says no, ask the pharmacist to call the insurer’s pharmacy help line. Most issues get resolved within 10 minutes.
Can I use GoodRx with Medicare?
Yes, but only if the GoodRx price is lower than your Medicare copay. Medicare rules say you can’t combine coupons with your plan’s price. But you can choose to pay cash with GoodRx instead of using your Medicare benefit. Just tell the pharmacist: “I’m paying cash today.” That’s legal and common.
Why do drug prices change so much between pharmacies?
Pharmacies negotiate different prices with drug distributors. Big chains like Walmart and Costco often have lower cash prices because they buy in bulk. Independent pharmacies may charge more. GoodRx shows you the lowest price nearby. Always check before you pay.
Are there free or low-cost alternatives to expensive brand-name drugs?
Yes. For most chronic conditions-diabetes, high blood pressure, cholesterol, depression-there are generic versions that work just as well. Even for newer drugs, biosimilars (similar to biologics) are now available and cost 15-30% less. Ask your doctor or pharmacist: “Is there a generic or biosimilar version?”
What if I can’t afford my meds even with insurance?
Contact the drug manufacturer. Most have patient assistance programs. You can also call 211 (free hotline) or visit NeedyMeds.org. Nonprofits like the Patient Advocate Foundation help with copay assistance and appeals. Don’t give up-help exists.
Susannah Green
Okay, but can we talk about how pharmacies are literally *designed* to confuse you? I had a 30-day script for metformin that cost $4 with GoodRx, but my insurance said $42-so I paid cash. Then the pharmacist acted like I’d committed a crime. Like, I’m not trying to game the system-I’m trying not to sleep on the couch next month. Why does this have to be so hard?!



Write a comment