When you’re seeing more than one doctor, pharmacist, or specialist, keeping track of your medications isn’t just a chore-it’s a safety issue. Every year, medication communication failures lead to avoidable hospital visits, dangerous drug interactions, and even deaths. If you’re taking five or more medications, or if you’ve been treated by multiple providers in the past year, you’re at higher risk. The good news? You don’t have to wait for your providers to fix this. You can take control-right now.
Why Medication Communication Breaks Down
Imagine this: Your cardiologist prescribes a new blood thinner. Your rheumatologist adds an anti-inflammatory. Your primary care doctor adjusts your diabetes med. None of them know what the others prescribed. That’s not a rare mistake-it’s the norm in fragmented care systems.
According to a 2022 NIH study, patients with three or more providers are over three times more likely to have conflicting medications. Specialists initiate 41% of new prescriptions without checking with your main doctor. And here’s the kicker: 83% of patients think their providers talk to each other. They don’t.
Electronic health records (EHRs) were supposed to fix this. But a 2023 CMS report found that 43% of providers struggle to access full medication histories across different systems. If your cardiologist uses one hospital’s EHR and your pharmacist uses another, they’re working in the dark. And when systems don’t talk, patients pay the price.
The Four Essential Elements of a Medication List
Stop relying on memory. Stop trusting sticky notes. Start using a real, updated list-with four key details for every medication:
- Name (brand and generic, if applicable)
- Dosage (e.g., 10 mg, 500 mg)
- Frequency (e.g., once daily, twice a week)
- Purpose (e.g., "for high blood pressure," "for arthritis pain")
This isn’t optional. Happier at Home’s 2022 clinical guidelines show that patients who use this format reduce medication errors by 37%. Keep it in your wallet, on your phone, and give a copy to every provider-even the nurse who checks your vitals.
Update it every time something changes. If your pharmacist switches you from a brand-name drug to a generic, add that. If your doctor cuts a dose, update it. If you stop a med because of side effects, cross it out. This list is your lifeline.
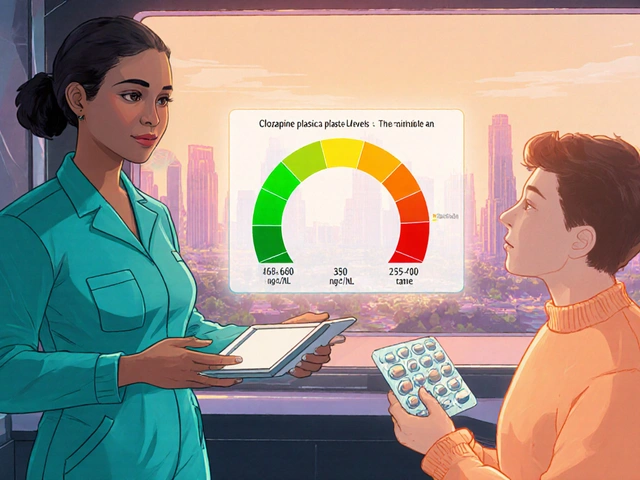
Who Should Be on Your Care Team
You’re not just a patient-you’re the captain of your care team. That means knowing who to talk to and when.
- Your primary care provider should be your central hub. They see the full picture. Make sure they have your complete list.
- Your pharmacist is your best ally. They’re trained to spot interactions. Many pharmacies now offer free Medication Therapy Management (MTM) services. Ask for it.
- Specialists often focus on one issue. Don’t assume they know what else you’re taking. Always say: "I’m on these other meds. Can you check if this new one conflicts?"
- Nurses and care coordinators in clinics or hospitals often manage transitions. Give them your list when you’re admitted or discharged.
Research from Asteroid Health in 2023 found that patients who worked directly with clinical pharmacists had 32% higher medication adherence and 63% more confidence in their regimen. That’s not magic-it’s communication.
How to Talk to Your Providers-Without Sounding Accusatory
You don’t need to argue. You just need to ask the right questions.
Before every appointment, write down:
- What side effects you’ve noticed (even small ones)
- Any changes in your sleep, mood, appetite, or energy
- Whether you’ve missed doses or skipped meds
Then, say this:
"I’ve been keeping a list of all my meds. I want to make sure everything I’m taking still makes sense together. Can we go through it?"
This opens the door without putting anyone on the defensive. Studies show that when patients use this approach, providers are 50% more likely to review all medications-not just the one they came in for.
Use the Teach-Back Method: After your provider explains a new med, say, "Just to make sure I got it right-you’re saying I take this once a day with food because it helps with stomach upset, right?" That simple trick reduces misunderstandings by 45%, according to the AHRQ.
Track Your Body’s Response
Doctors can’t read your mind. But a journal can.
Start a simple log: date, medication, dose, and what you felt that day. Did you feel dizzy after taking your new blood pressure pill? Did your knee pain get worse after starting the new painkiller? Did you sleep worse after the antibiotic?
University of California San Francisco’s 2023 study found that patients who tracked symptoms this way had 22% fewer adverse drug events. You’re not just reporting side effects-you’re giving your providers data they can’t get otherwise.
Keep it digital (a notes app works) or on paper. The key is consistency. Even 30 seconds a day adds up.
When You’re in the Hospital
Transitions between care settings are the most dangerous moments. A 2022 study found that 56% of hospital transitions involve medication reconciliation errors-and 28% of those are potentially harmful.
Before you’re discharged, insist on this:
- A full review of all your meds by a pharmacist
- A written update to your primary care provider
- A copy of your updated medication list in your hands
Ask: "Who will make sure my primary doctor gets this?" Don’t assume it’s done. If they say "We’ll send it," ask for a phone number to follow up.
What Works: Integrated Care Systems
Not all systems are broken. Accountable Care Organizations (ACOs) and integrated health networks show real results. CMS data from 2022 shows ACO patients had 27% fewer medication-related hospital readmissions.
Why? Because they have:
- Shared EHRs across providers
- Pharmacists embedded in care teams
- Regular team huddles to review complex cases
One Medicare beneficiary in a CMS patient story credited her ACO’s care team with spotting five dangerous interactions across her three specialists. "They caught what no one else did," she said.
If you’re in an ACO or similar system, use it. Ask if you have a care coordinator. Ask if your meds are reviewed quarterly. You’re paying for this service-demand it.
What’s Coming Next
Change is happening. By 2025, 78% of independent pharmacies will offer formal medication therapy management services. AI tools at places like Mayo Clinic are cutting medication review time from 15 minutes to under a minute. The Commonwealth Fund estimates every $1 spent on better communication returns $7.30 in saved hospital costs.
But none of this matters if you’re not involved. The system won’t fix itself. You have to be the glue.
Start Today: Your Action Plan
Here’s what to do this week:
- Write down every medication you’re taking-name, dose, frequency, purpose.
- Update it with your pharmacist. Ask if they can help you review it.
- Bring your list to your next doctor’s appointment. Say: "Can we go through this together?"
- Start a simple symptom log. Just note changes in how you feel.
- Ask your primary care provider: "Who should I call if I have a question about my meds?" Get their direct number.
You don’t need permission. You don’t need to be an expert. You just need to be consistent. One list. One conversation. One journal. That’s all it takes to prevent a mistake that could change your life.
What should I do if my doctors prescribe conflicting medications?
If you notice conflicting medications-like two drugs that interact or duplicate effects-don’t stop taking anything. Contact your pharmacist or primary care provider immediately. They can review the list, contact the other providers, and suggest safer alternatives. Never adjust doses or stop meds on your own without professional advice.
Can my pharmacist really help me with multiple providers?
Yes. Pharmacists are trained to spot drug interactions and are often the only provider who sees all your prescriptions. Many pharmacies offer free Medication Therapy Management (MTM) services, where they review your entire regimen, contact your doctors, and create a clear action plan. Ask for it-no referral needed.
Why do specialists often prescribe without consulting my primary doctor?
Specialists focus on one condition, and many don’t have access to your full medication history. EHR systems often don’t talk to each other, and there’s no legal requirement for them to coordinate. That’s why you need to be the bridge-always bring your list, ask if they checked your other meds, and follow up.
How often should I update my medication list?
Update it every time you start, stop, or change a medication-even if it’s temporary. Also update it after every hospital visit, ER trip, or pharmacy refill. Keep it current. A 2023 Tulane study found patients with up-to-date lists had 37% fewer medication errors.
What if I’m too overwhelmed to manage this?
You’re not alone. Many patients feel this way. Ask your primary care provider if they have a care coordinator or social worker who can help. Some clinics offer medication management support. You can also ask a trusted family member to help you update your list or attend appointments with you. It’s okay to ask for help-it’s part of staying safe.