When treating patients with treatment‑resistant schizophrenia, Clozapine is a second‑generation antipsychotic that blocks dopamine D2 receptors and multiple serotonin receptors. It is the only medication shown to lower suicide risk in this group, but its narrow safety window means clinicians must keep a close eye on blood concentrations.
Quick Takeaways
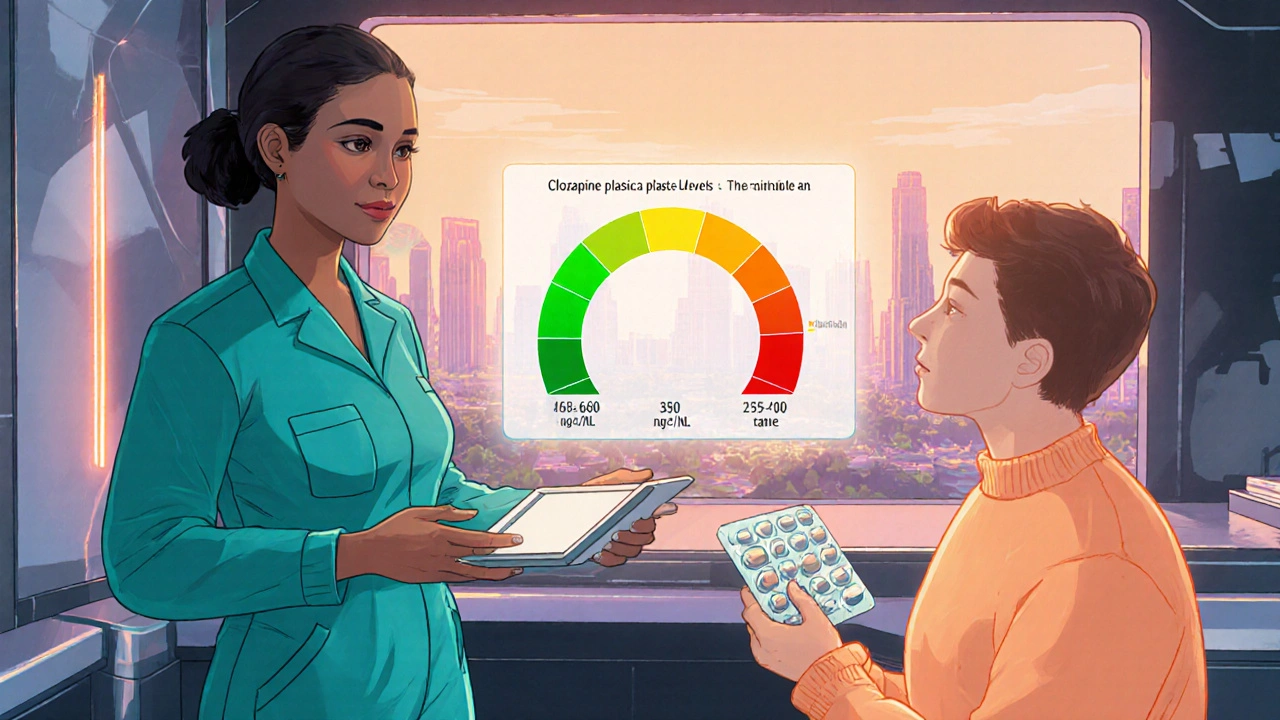
- Therapeutic plasma levels of clozapine are 350‑600 ng/mL; below this range the drug may be ineffective.
- Levels above 1000 ng/mL raise the risk of seizures, myocarditis, and severe sedation.
- Smoking, caffeine, and concurrent drugs that affect CYP1A2 can swing levels dramatically.
- Blood draws should be done as a trough sample (just before the next dose) and repeated after any dosage change.
- Using a simple checklist helps patients and prescribers stay on track with monitoring and dose adjustments.
Why Blood‑Level Monitoring Matters
Unlike many oral medications, clozapine’s efficacy and toxicity are tightly linked to its plasma concentration. Studies from the early 2000s to today show that patients who stay within the therapeutic window experience fewer relapses and a lower incidence of agranulocytosis‑related complications. In contrast, sub‑therapeutic levels often translate into persistent psychotic symptoms, while supratherapeutic levels can trigger seizures, severe sedation, and cardiac events.
Because the drug’s half‑life varies from 12 to 24 hours depending on metabolism, a single dose adjustment can result in a delayed spike or dip. Regular monitoring catches these shifts before they become clinically evident, allowing timely dose titration.
Therapeutic Range and Target Concentrations
The consensus therapeutic window for clozapine is 350‑600 ng/mL (nanograms per milliliter). Below 350 ng/mL, the odds of symptom control drop by roughly 30 %. Above 600 ng/mL, the probability of side‑effects rises sharply, with a marked increase in seizure risk once the level exceeds 1000 ng/mL.
| Category | Plasma Level (ng/mL) | Clinical Implication |
|---|---|---|
| Sub‑therapeutic | < 350 | Reduced efficacy; possible psychotic relapse |
| Therapeutic | 350‑600 | Optimal symptom control with manageable side‑effects |
| High‑risk | 600‑1000 | Increased sedation, orthostatic hypotension, mild‑to‑moderate seizures |
| Critical | > 1000 | Severe seizures, myocarditis, possible fatal outcomes |
Factors That Influence Clozapine Levels
Several variables push plasma concentrations up or down. Understanding them helps clinicians anticipate changes and adjust dosing proactively.
- CYP1A2 activity: Clozapine is metabolized primarily by the CYP1A2 enzyme. Inducers (e.g., smoking, carbamazepine) lower levels, while inhibitors (e.g., fluvoxamine, ciprofloxacin) raise them.
- Smoking status: Each cigarette can increase CYP1A2 activity by 10‑15 %, often requiring a 25‑50 % dose increase in smokers.
- Caffeine intake: Heavy coffee consumption competes for CYP1A2, modestly raising clozapine concentrations.
- Age and liver function: Elderly patients or those with hepatic impairment clear the drug slower, necessitating lower initial doses.
- Genetic polymorphisms: Certain CYP1A2 alleles (e.g., *1F) lead to rapid metabolism, while *1C results in slower clearance.
- Concurrent medications: Drugs that inhibit or induce CYP1A2 (e.g., omeprazole, rifampin) can swing levels dramatically.
Because these factors often change over time-patients quit smoking, start new meds, or develop liver disease-regular clozapine monitoring becomes a moving target that must be reassessed every few weeks.
When and How to Collect Blood Samples
The most reliable measurement is a trough level taken just before the next scheduled dose. This timing captures the lowest concentration and reflects steady‑state pharmacokinetics after at least five half‑lives (roughly 5‑7 days) of consistent dosing.
- Schedule the draw for the same time of day each week (typically morning before the morning dose).
- Instruct the patient to avoid caffeine and nicotine for at least two hours before the draw, if possible.
- Use a lithium heparin tube; plasma is required, not serum.
- Label the sample with patient ID, date, and time of last dose.
- Send the specimen to a certified laboratory that offers high‑performance liquid chromatography (HPLC) or mass‑spectrometry assays.
If a dose change occurs, repeat the level after five days to confirm the new steady state. During the initiation phase (first 2‑3 weeks), weekly monitoring is recommended; later, monthly checks are sufficient for stable patients.
Interpreting Results and Adjusting Dosage
Take the reported concentration and compare it to the therapeutic window. Below are typical actions:
- Result < 350 ng/mL: Increase the daily dose by 25 mg increments, re‑measure after five days.
- Result 350‑600 ng/mL: Maintain current dose; focus on adherence and side‑effect monitoring.
- Result 600‑1000 ng/mL: Assess for sedation, orthostatic hypotension, or mild seizures. Consider a 10‑20 % dose reduction and evaluate contributing factors (e.g., new CYP1A2 inhibitor).
- Result > 1000 ng/mL: Immediate dose reduction by 30‑50 % or temporary discontinuation. Treat any seizures with benzodiazepines and monitor cardiac enzymes for myocarditis.
Never adjust the dose based solely on a single outlier value; confirm with a repeat draw to rule out laboratory error or recent lifestyle changes.
Practical Checklist for Clinicians and Patients
- Document baseline plasma level before any dose change.
- Review smoking status, caffeine consumption, and any new prescriptions at each visit.
- Schedule trough blood draws at consistent times.
- Maintain a log of all plasma levels, doses, and side‑effects.
- Educate patients on the signs of toxicity (seizures, severe sedation, chest pain) and advise them to call immediately.
- Re‑assess dosing after any major lifestyle change (e.g., quitting smoking).
Following this routine transforms clozapine from a high‑risk drug into a precisely managed therapy that saves lives.
Frequently Asked Questions
How often should I get my clozapine blood level checked?
During the first month, weekly checks are advised. Once a stable therapeutic level is reached, monthly monitoring is usually enough unless the dose changes or new medications are added.
Can I skip a blood test if I feel fine?
No. Clozapine toxicity can develop without obvious symptoms. Missing a test may let dangerous levels go unnoticed, especially after a dosage change or lifestyle shift.
What should I do if my level is above 1000 ng/mL?
Contact your prescriber immediately. They will likely lower the dose by 30‑50 % and monitor you for seizures or cardiac issues. Do not adjust the dose on your own.
Does smoking really affect clozapine levels?
Yes. Each cigarette can boost CYP1A2 activity, lowering the drug’s plasma concentration by up to 30 %. If you quit smoking, your doctor will likely reduce the dose to avoid toxicity.
Are there any food or drink restrictions?
Heavy caffeine intake can slightly raise clozapine levels because both compete for CYP1A2. Moderation (no more than 2‑3 cups of coffee a day) is recommended, especially around blood draws.
By treating clozapine monitoring as a routine part of care, patients gain the full therapeutic benefit while minimizing life‑threatening side effects.
Grace Silver
Monitoring clozapine is like keeping a lighthouse on a stormy sea. The drug can save lives but it also hides dangers under its veil. Blood levels give us the map that shows where the safe harbor lies. Without regular checks a patient may drift into toxicity without warning. The therapeutic window of 350 to 600 nanograms per milliliter is a narrow bridge. A step too far on either side can cause seizures or loss of symptom control. Factors such as smoking caffeine and other meds constantly shift that bridge. That is why clinicians must treat each draw as a checkpoint on a journey. The timing of a trough sample just before the dose captures the lowest point. It lets us see the true steady state after the drug has settled. Adjusting dose after a single outlier is unwise; confirmation through a repeat draw is essential. Patients themselves become partners when they log their smoking habits and caffeine intake. Education about signs of toxicity turns fear into empowerment. In my experience the simple checklist becomes a compass that guides both doctor and patient. When the process is routine the drug transforms from a high risk weapon into a precise instrument for recovery.
Tamara Tioran-Harrison
It is truly astonishing how a drug with such a narrow therapeutic index can be prescribed without a daily blood test, as if physicians were playing roulette with patients. One would expect a more rigorous protocol, yet the reality feels like a bureaucratic oversight. :)
Brett Witcher
The pharmacokinetic profile of clozapine demands a level of analytical vigilance that is seldom afforded in routine practice. A precise trough measurement, taken under controlled conditions, yields data of undeniable clinical relevance. Variability introduced by CYP1A2 modulation is not a peripheral concern but a central determinant of therapeutic success. Consequently, dose adjustments should be predicated upon a series of corroborative assays rather than isolated readings. In sum, the discipline of systematic monitoring is indispensable to harnessing clozapine's therapeutic potential.
Bianca Larasati
Listen up team! The battle against relapse is won in the lab, not just in the clinic. Every trough draw is a victory flag that tells us we’re still on course. When the numbers dance within range, we can celebrate the small triumphs. If they slip, we rally, adjust, and keep the momentum alive.
Abhinav B.
Hey folks, let me tell you why this is not just some fancy lab thing. In my country we see patients who smoke a lot and then quit cold turkey – their levels go thru the roof! So doctors need to be on top of these changes, otherwise you get seizures and bad outcomes. Also, be careful with coffee, it can push the levels up a noticable amount. Keep the monitoring regular and you will avoid many scary side effects.
Abby W
Got it, will keep the checklist handy 😊
Lisa Woodcock
Thanks for the reminder! It really helps to have a clear plan so patients don’t feel lost. I always make sure to explain each step and answer any concerns they might have.
krishna chegireddy
They don't want you to know that the labs are sometimes rigged to hide the real numbers. Imagine the chaos if everyone saw the true spikes – the system would crumble. That's why we must stay alert and question every result. Trust no one, verify everything.
Tamara Schäfer
Thinking about clozapine monitoring makes me reflect on how small habits shape big outcomes. Even a tiny change like cutting back on coffee can tip the balance toward safety. It's encouraging to see that patients can actively participate in their own care. With patience and proper guidance, the therapeutic window becomes reachable. Keep believing in the process and the results will follow.





Write a comment