What Is Pleural Effusion?
When fluid builds up between the layers of tissue lining your lungs and chest wall, that’s called a pleural effusion. It’s not a disease on its own-it’s a sign something else is wrong. Think of it like swelling around your lungs. That extra fluid makes it harder for your lungs to expand fully, so you feel short of breath, especially when you’re active or lying down. Some people also get a sharp chest pain when they breathe in, or a dry cough. But here’s the thing: you might not feel anything at all. Small effusions often show up on a chest X-ray done for another reason.
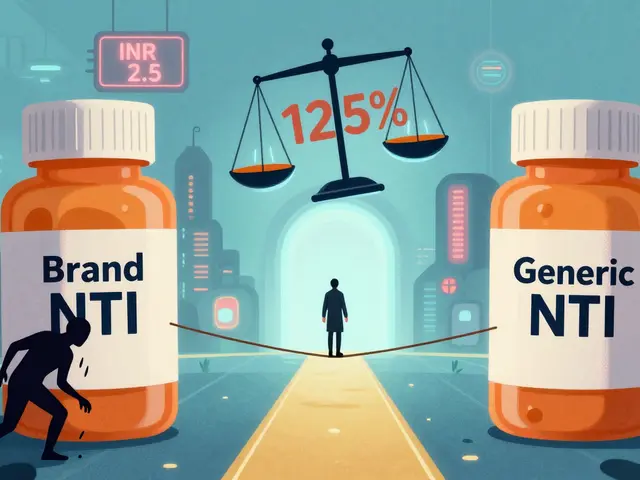
Doctors classify pleural effusions into two main types: transudative and exudative. Transudative means fluid is leaking because of pressure changes-usually from heart failure, liver disease, or kidney problems. Exudative means inflammation or infection is making blood vessels leaky. This type is more serious and often tied to pneumonia, cancer, or blood clots in the lungs.
What Causes Pleural Effusion?
The cause tells you how to treat it. If you get it wrong, the fluid comes back-and fast.
Half of all cases come from congestive heart failure. When the heart can’t pump well, pressure builds up in the blood vessels around the lungs, and fluid seeps out. That’s why people with heart failure often wake up gasping for air at night. Liver cirrhosis and nephrotic syndrome are less common but still important causes. In cirrhosis, low protein levels in the blood pull fluid into the pleural space. In nephrotic syndrome, the kidneys leak protein, which does the same thing.
Exudative effusions are trickier. Pneumonia is the biggest culprit, causing 40-50% of these cases. When lung infection spreads to the pleural space, it triggers inflammation and thick fluid buildup. If not drained, it can turn into empyema-pus in the chest-which needs surgery. Cancer is the second leading cause, responsible for 30-40% of exudative cases. Lung cancer, breast cancer, and lymphoma often spread to the pleura. Tuberculosis still causes effusions in some regions, though it’s rare in places like Australia.
Less common but dangerous causes include pulmonary embolism (a blood clot in the lung), autoimmune diseases like rheumatoid arthritis, and even after heart surgery. About 15-20% of people who have bypass surgery develop a pleural effusion. Most go away on their own, but if it’s large or lasts too long, it needs attention.
How Is It Diagnosed?
It starts with listening. Your doctor will tap on your chest and listen with a stethoscope. Dull sounds mean fluid is there. But that’s not enough. You’ll need an ultrasound or chest X-ray to confirm. Ultrasound is now the gold standard-it shows exactly how much fluid is there and where to stick the needle.
The real key is fluid analysis. A procedure called thoracentesis removes a small sample. That fluid gets tested for protein, lactate dehydrogenase (LDH), glucose, pH, and cells. This is where Light’s criteria come in. If the fluid protein is more than half the blood protein, or LDH is over two-thirds of the blood level, it’s exudative. These rules are 99.5% accurate. If the fluid pH is below 7.2, or glucose is under 60 mg/dL, it’s likely infected or cancer-related.
Cytology-looking for cancer cells under the microscope-finds malignancy in about 60% of cases. But sometimes, you need more than one sample. That’s why doctors don’t stop at one test. They look at the whole picture: your symptoms, your history, your imaging, and the fluid results.

What Is Thoracentesis?
Thoracentesis is the procedure to drain fluid from the pleural space. It’s simple, quick, and done under local numbing. You sit upright, leaning forward. The doctor finds the right spot-usually between the 5th and 7th ribs on your side-and uses ultrasound to guide the needle. That’s critical. Without ultrasound, complications like a collapsed lung happen in nearly 19% of cases. With it? Down to 4%.
For diagnosis, they take 50-100 mL. For relief, they can take up to 1,500 mL in one go. But they don’t just drain as much as possible. Too much too fast can cause re-expansion pulmonary edema-a rare but serious swelling in the lung after it re-inflates. That’s why doctors use pleural manometry now. If pressure drops below 15 cm H₂O during drainage, you’re safe. If it goes higher, they stop.
Complications are rare but real. Pneumothorax (collapsed lung) happens in 6-30% of unguided procedures. Hemorrhage occurs in 1-2%. Re-expansion edema is under 1%. That’s why this isn’t a DIY procedure. It needs training. Studies show you need at least 25 supervised procedures to get good at it.
How Do You Stop It From Coming Back?
Draining the fluid gives you relief-but it doesn’t fix the problem. The fluid comes back if the root cause isn’t treated.
If it’s from heart failure, the answer is medicine. Diuretics like furosemide help the kidneys flush out extra fluid. ACE inhibitors and beta-blockers improve heart function. When doctors use NT-pro-BNP levels to guide treatment, recurrence drops from 40% to under 15% in three months.
If it’s from pneumonia, antibiotics are the first step. But if the fluid is thick, low in pH, or has bacteria, you need to drain it fully. If you don’t, 30-40% of cases turn into empyema. That means surgery to clean out the chest.
Malignant effusions are the toughest. After one thoracentesis, half of them come back within 30 days. That’s why doctors don’t just drain and wait. They offer pleurodesis-a procedure that sticks the lung to the chest wall so fluid can’t collect. Talc is the most common agent. It works in 70-90% of cases. But it’s painful. Sixty to eighty percent of patients need strong pain meds afterward.
Now, there’s a better option: indwelling pleural catheters. These are small tubes left in place for weeks. You drain the fluid yourself at home, a little at a time. Success rates are 85-90% at six months. Hospital stays drop from over a week to just two days. For people with advanced cancer, this is life-changing. It means less pain, more control, and fewer hospital visits.

What Doesn’t Work?
Not every effusion needs to be drained. If it’s small and you feel fine, doctors now advise watching and waiting. A 2019 JAMA study found that 30% of thoracenteses done for tiny, asymptomatic effusions gave no benefit. You just get the risk of complications for nothing.
And chemical pleurodesis isn’t recommended for non-cancer causes. It doesn’t work for heart failure, liver disease, or kidney problems. You’re not patching the hole-you’re just sealing the leak. The fluid finds another way out. That’s why guidelines now say: fix the heart, fix the liver, treat the infection. Don’t just glue the pleura shut.
What’s New in 2026?
Recent advances are shifting how we think about this condition. The focus is no longer just on removing fluid-it’s on matching the treatment to the cause.
For cancer patients, treatment is now personalized. If you have lung cancer with a specific mutation, targeted therapy can shrink the tumor and reduce fluid buildup without pleurodesis. Survival rates have improved from 10% to 25% over the last decade because of this.
Pleural manometry is becoming standard. It’s not just about how much fluid you take out-it’s about how fast and how safely. Pressure monitoring prevents re-expansion edema, which used to be a surprise complication.
And the big shift? Indwelling catheters are now first-line for malignant effusions, not a last resort. They’re cheaper, safer, and better for quality of life. The American Thoracic Society updated its guidelines in 2020 to reflect this. The European Respiratory Society followed in 2023.
What Should You Do If You Have This?
If you’re diagnosed with pleural effusion, don’t panic. But don’t ignore it either. Ask your doctor:
- Is this transudative or exudative?
- What’s the most likely cause?
- Do I need fluid analysis?
- Will I need thoracentesis, and will it be ultrasound-guided?
- What’s the plan if it comes back?
Don’t accept a simple drainage without knowing why it happened. That’s like fixing a leaky roof without checking for termites. The fluid will come back. And next time, it might be worse.
Bianca Leonhardt
This is why most doctors are lazy. They drain the fluid like it's a quick fix and never ask why it's there. You think a diuretic solves heart failure? Nah. It just delays the inevitable. People die because no one wants to deal with the root cause. Just patch the leak and call it a day.
Bobbi-Marie Nova
lol i got pleural effusion last year and my doc just said 'drink less water'... i swear i thought he was joking. turns out he meant 'take your diuretics' but yeah... i still think he's a goofball.
Travis Craw
i didnt know thoracentesis needed ultrasound guidance. my doc just stuck a needle in without even checking. i was lucky it didnt puncture my lung. kinda scary when you think about it.
Isabella Reid
I’ve had two episodes of this-both after pneumonia. The first time they drained me and I felt like a new person. The second time, they used the indwelling catheter. Honestly? Best decision ever. I drained it at home while watching Netflix. No hospital stays. No pain meds. Just me, my cat, and a little syringe. Life-changing.
swarnima singh
they say pleurodesis works 70-90% of the time but what they dont tell you is that the pain is like someone is slowly grinding your ribs with a cheese grater. i screamed for three days. and then the fluid came back anyway. why do they even do this? its just torture with a fancy name.
Jody Fahrenkrug
my aunt had this after her bypass. doc said it was normal, just watch it. two months later she was back in ER with a massive buildup. turns out they never did fluid analysis. just assumed. now she’s on a catheter. i wish they’d listened to her when she said something felt off.
kanchan tiwari
this is all a lie. the government and big pharma don’t want you to know that pleural effusion is caused by chemtrails. they use the 'heart failure' excuse to make you take pills that keep you dependent. the real cure? Himalayan salt and breathwork. but they’ll never tell you that because it’s free.
john Mccoskey
The entire medical paradigm around pleural effusion is fundamentally flawed. Light’s criteria are statistically valid but clinically overused. The assumption that protein and LDH ratios dictate etiology ignores the dynamic interplay of systemic inflammation, endothelial permeability, and lymphatic drainage dynamics. Most clinicians don’t understand the Frank-Starling mechanism’s role in transudative formation, and yet they’re the ones ordering thoracenteses. The push for indwelling catheters is a cost-cutting measure disguised as patient-centered care. Pleurodesis isn’t outdated-it’s underutilized in non-malignant cases because of poor training. And let’s not even get started on how rarely pleural manometry is implemented despite its proven safety profile. We’re treating symptoms like they’re the disease.
Ryan Hutchison
in america we overtest everything. in my country we just treat the symptoms and move on. why waste money on ultrasounds and fluid analysis? if you’re short of breath, drain it. if you’re still short of breath, drain it again. simple. no need for all this fancy science nonsense.
Melodie Lesesne
i had a friend with lung cancer who got the indwelling catheter. she said it gave her back her life. she could go to her book club, cook dinner, even travel to see her grandkids. no more hospital trips. no more needles. just a little drain every few days. it’s not glamorous but it’s real. and honestly? that’s what matters.
Corey Sawchuk
i never knew about re-expansion edema until i read this. my uncle had a huge drain and then got really sick after. they said it was pneumonia but i always wondered if it was that thing. glad to see they’re monitoring pressure now. that’s smart
Rob Deneke
if you’ve got this and you’re not getting ultrasound-guided thoracentesis you’re getting ripped off. period. i’ve seen too many people get pneumothorax because someone was too lazy to use the machine. it’s not hard. it’s not expensive. just do it right.
Riya Katyal
oh so now we’re supposed to believe that talc pleurodesis is the gold standard? lol. i bet the pharmaceutical reps paid off every guideline writer. next they’ll say aspirin cures cancer.
Allen Davidson
You know what’s wild? This whole post is basically a masterclass in how to treat pleural effusion right. Most docs skip half this stuff. If you’re reading this and your doctor hasn’t mentioned Light’s criteria or manometry? Ask for it. Don’t settle. You’re not just a patient-you’re your own best advocate.



Write a comment