PONV Risk Calculator
Calculate Your Post-Surgery Nausea Risk
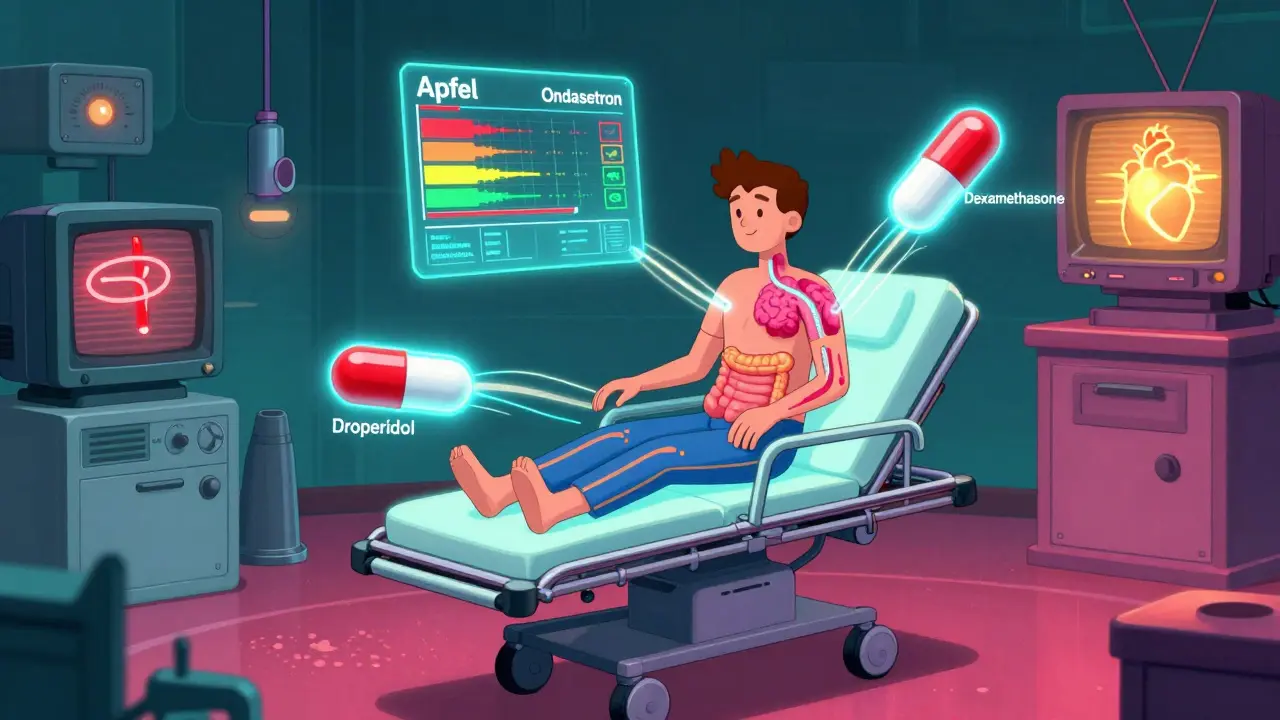
This tool calculates your Apfel risk score for post-operative nausea and vomiting (PONV).
When you’re recovering from surgery, chemo, or even a simple painkiller, nausea can feel like the worst part of the whole experience. It’s not just uncomfortable-it can delay healing, make you skip meals, or even send you back to the hospital. The good news? There are effective medicines called antinausea meds-or antiemetics-that can stop it. But not all of them work the same way, and picking the wrong one can mean wasted money, side effects, or even serious risks. So how do you choose safely?
Why Some Nausea Won’t Go Away with Just Ginger Tea
Nausea from meds isn’t like motion sickness or morning sickness. It’s triggered by how drugs interact with your brain and gut. Opioids like morphine mess with your brain’s vomiting center. Chemo drugs flood your system with serotonin, which tells your gut to revolt. Anesthesia affects multiple pathways at once. That’s why over-the-counter remedies often fail. You need targeted drugs that block the right signals.The Seven Main Types of Antiemetics and How They Work
There are seven classes of antiemetics, each with a different job. Think of them like specialized tools for different jobs:- 5-HT3 antagonists (ondansetron, granisetron): Block serotonin in your gut and brainstem. Best for chemo and post-surgery nausea. Ondansetron works in about 65-75% of cases.
- Dopamine antagonists (droperidol, metoclopramide): Quiet the brain’s vomiting center. Droperidol is cheap, fast, and works well even in opioid-tolerant patients. Metoclopramide also speeds up stomach emptying-useful if your nausea comes from slow digestion.
- Corticosteroids (dexamethasone): Not a direct anti-nausea drug, but it boosts the effect of others. Takes 4-5 hours to kick in, so it’s best used with something faster.
- Antihistamines (promethazine): Good for motion sickness, but weak against drug-induced nausea. Can make you drowsy.
- Anticholinergics (scopolamine patch): Used for travel nausea. Too slow for acute cases and not great for surgery or chemo.
- Sedatives (lorazepam, olanzapine): Not first-line, but olanzapine has shown surprising results in cancer patients who don’t respond to other drugs.
- Opioid antagonists (nalmefene): Rarely used. Only for specific cases where opioids are the clear trigger.
What Works Best for Post-Surgery Nausea (PONV)?
About 30% of people feel sick after surgery. That’s 3 in every 10. The risk goes up if you’re female, don’t smoke, have had nausea before, or need opioids afterward. The Apfel score helps doctors figure out your risk level:- 0-1 risk factors: Skip prophylaxis. Treat only if nausea hits.
- 2 risk factors: Use one antiemetic. Ondansetron 4 mg IV or droperidol 0.625 mg IV are top choices.
- 3-4 risk factors: Use two. Droperidol + dexamethasone is the most proven combo. Studies show it cuts nausea by more than half.

Chemo Nausea? It’s a Different Battle
Chemotherapy can cause nausea right away (acute) or days later (delayed). For acute nausea, 5-HT3 blockers like ondansetron or granisetron are standard. For delayed nausea, adding dexamethasone helps. But if you’ve tried everything and still feel sick, newer drugs like netupitant/palonosetron (Akynzeo) are changing the game. In trials, they gave a 75% complete response rate-meaning no vomiting and no need for rescue meds-compared to 63% with older combos. New options like intranasal ondansetron (Zuplenz) are helpful for patients who can’t swallow pills after chemo. It works just as well as IV, with 89% bioavailability. No needles, no IV lines-just a spray in the nose.What About Side Effects? Don’t Ignore the Risks
Every drug has trade-offs:- Ondansetron: Can cause headaches (32% of users), dizziness, or abnormal vision. Rarely, it can prolong the QT interval-especially in people with heart conditions or those taking other QT-prolonging drugs. The FDA warns against using it in people with congenital long QT syndrome.
- Droperidol: Very safe at low doses (0.625-1.25 mg). But above 1.25 mg, it can cause QT prolongation. That’s why hospitals require ECG monitoring for higher doses.
- Metoclopramide: Can cause muscle spasms, restlessness, or even a condition called akathisia-especially in older adults. One ER doctor reported 8% of elderly patients got severe agitation on 10 mg. That’s why many now use olanzapine 2.5-5 mg instead.
- Dexamethasone: Safe short-term, but long-term use can raise blood sugar, cause insomnia, or weaken bones.
Real-World Insights: What Nurses and Anesthesiologists Say
Published studies tell you what *should* work. Real practitioners tell you what *does* work:- At Massachusetts General Hospital, combining dexamethasone 4 mg with ondansetron 4 mg cut rescue meds by 32% in opioid-induced nausea cases.
- On Reddit’s r/Anesthesiology, multiple anesthesiologists say droperidol 0.625 mg is their go-to for opioid-tolerant patients-faster, cheaper, and less sedating than ondansetron.
- One ER team switched from metoclopramide to olanzapine for elderly patients after seeing too many cases of akathisia.
- Patients on Drugs.com praise ondansetron for working in 15 minutes-but many say the headache is worth it.
Cost Matters-Even in Hospitals
A single case of uncontrolled PONV costs an extra $1,086 in hospital time, extra meds, and staff effort. That’s why smart hospitals run antiemetic stewardship programs. They track which drugs are used, when, and how often they fail. One hospital cut costs by 20% by switching from branded ondansetron to generic, and replacing high-cost combo drugs with droperidol + dexamethasone where appropriate. The global antiemetic market is worth $5.8 billion. But 73% of health systems now have rules to avoid overuse. Why? Because 30-40% of antiemetic doses are given to people who don’t even need them-low-risk patients getting meds they won’t benefit from.What’s New and What’s Coming
The future is personalized. Researchers are studying genetic differences-like CYP2D6 variants-that affect how people metabolize ondansetron. Some people break it down too fast; others too slow. In the next five years, we may see genetic tests guiding antiemetic choice. NK-1 receptor antagonists like rolapitant are already helping with delayed chemo nausea, with 78% efficacy. Intranasal and oral dissolving forms are making administration easier. And combination pills like Akynzeo are becoming standard for high-risk chemo patients.Bottom Line: How to Choose Safely
1. Match the drug to the cause. Chemo? Start with 5-HT3 blocker. Post-op? Droperidol or ondansetron. Slow stomach? Metoclopramide. 2. Use risk scores. Don’t give antiemetics to everyone. Use the Apfel score. If you have 0-1 risk factors, wait and treat only if needed. 3. Combine wisely. One drug often isn’t enough for high-risk patients. Droperidol + dexamethasone is proven, safe, and cheap. 4. Watch the side effects. Don’t use metoclopramide in the elderly. Avoid high-dose ondansetron in people with heart issues. Monitor ECG if using droperidol above 1.25 mg. 5. Think cost and access. Generic ondansetron, droperidol, and dexamethasone are all under $2 per dose. Newer drugs cost hundreds. Use them only when needed. Nausea doesn’t have to be part of your recovery. With the right antiemetic, chosen based on your risk, your meds, and your body’s needs-you can get through it without suffering.What’s the best antiemetic for post-surgery nausea?
For most patients, droperidol (0.625-1.25 mg IV) or ondansetron (4 mg IV) are equally effective. Droperidol is cheaper and works faster, especially in opioid-tolerant patients. For high-risk patients (3-4 Apfel risk factors), combining droperidol with dexamethasone reduces nausea by more than half.
Is ondansetron safe for everyone?
No. Ondansetron can prolong the QT interval, which increases the risk of dangerous heart rhythms. Avoid it in people with congenital long QT syndrome, those taking other QT-prolonging drugs, or those with severe heart disease. Headaches are common (32% of users), but usually mild.
Why is droperidol not used more often?
Fear of side effects. Droperidol has a black box warning for QT prolongation-but only at doses above 1.25 mg. At the low doses used for nausea (0.625-1.25 mg), it’s very safe and often more effective than ondansetron. Many hospitals avoid it due to outdated concerns, not evidence.
Can I use promethazine for chemo nausea?
It’s not recommended. Promethazine works better for motion sickness and allergies. For chemo-induced nausea, 5-HT3 blockers like ondansetron are far more effective, with 65-75% success versus promethazine’s 40-50%.
What’s the cheapest effective antiemetic?
Dexamethasone ($0.25 per 8 mg dose) and droperidol ($0.50 per 0.625 mg dose) are the most cost-effective. Used together in high-risk patients, they provide better results than expensive 5-HT3 blockers like granisetron or netupitant/palonosetron.
How long does it take for dexamethasone to work?
Dexamethasone takes 4-5 hours to reach full effect. That’s why it’s never used alone for acute nausea. It’s best combined with faster-acting drugs like ondansetron or droperidol, especially for surgery or chemo.
Are there any new antiemetics on the horizon?
Yes. Intranasal ondansetron (Zuplenz) is now approved and works as well as IV. NK-1 antagonists like rolapitant are improving control of delayed chemo nausea. In the next few years, genetic testing may guide which drug works best for your body, making treatment truly personalized.
Kamlesh Chauhan
this whole thing is just pharma brainwashing
they want you hooked on drugs so you keep coming back
why not just drink ginger tea and pray like our ancestors did?
Emma Addison Thomas
Interesting breakdown. I've seen droperidol used in the UK for post-op nausea and it's remarkably effective-though the stigma around it is real. A shame, really, when the data supports its safety at low doses.
Mina Murray
ondansetron causes headaches? no shit. i got one so bad after chemo i thought my skull was splitting. but hey, at least i didn't vomit. also, dexamethasone made me feel like a zombie for three days. this whole system is broken.
Rachel Steward
Let’s be real: the entire antiemetic industry is a profit-driven circus. You have a $5.8 billion market built on suppressing symptoms instead of addressing root causes. Why not question why chemo causes nausea in the first place? Why not optimize the body’s own endogenous systems? Instead, we throw serotonin blockers at people like it’s a magic bullet. It’s not medicine-it’s chemical band-aids on a bullet wound. And don’t get me started on the ‘risk scores’-they’re just algorithms to justify prescribing. The real solution? Reduce chemo toxicity. But that wouldn’t make anyone rich.
Christine Joy Chicano
The fact that intranasal ondansetron has 89% bioavailability is mind-blowing. No IV, no needles, just a quick spray? That’s a game-changer for patients who are nauseated enough to gag at the sight of a syringe. I’ve seen people cry because they couldn’t swallow pills after chemo-this could restore dignity. Kudos to the researchers who pushed for this. It’s small, but it matters.
Adam Gainski
I work in a hospital pharmacy and we switched to generic ondansetron + dexamethasone for most PONV cases. Cut our costs by 30% without losing efficacy. Droperidol’s still underused though-nurses are scared of it because of old warnings. The data says it’s safe at 0.625 mg. We’ve given it to over 200 patients this year. Zero arrhythmias. Just quiet, effective nausea control.
Anastasia Novak
i can’t believe people still think dexamethasone is ‘safe short-term’. have you seen the mood swings? the insomnia? the way it turns you into a rage monster who yells at their cat at 3am? i took it after surgery and i hated myself for a week. this isn’t medicine-it’s emotional terrorism with a prescription label.
Jonathan Larson
The pursuit of pharmacological solutions must be balanced with ethical stewardship. While efficacy and cost are critical, we must not lose sight of the patient’s holistic experience. A drug that prevents vomiting but induces existential dread or cardiac risk may not be a true victory. Medicine, at its core, should alleviate suffering-not replace one form of distress with another. The future lies not only in molecular precision but in compassionate calibration.
Alex Danner
Droperidol at 0.625 mg is the unsung hero of post-op care. I’ve used it in the ER for opioid-induced nausea and it knocks it out faster than ondansetron. No sedation. No cost. Just pure, quiet relief. The fact that hospitals avoid it over a 20-year-old black box warning is criminal. We’re letting fear dictate clinical practice. Time to update the guidelines.
Kyle King
you know what’s really going on? the FDA and big pharma are hiding the truth. droperidol doesn’t cause QT prolongation at low doses-what it actually does is make patients too calm. they don’t want people calm. they want you anxious, dependent, and buying more pills. this whole antiemetic guide? it’s a distraction. the real cure is meditation and sunlight.




Write a comment