Medication Interaction Checker
Why This Matters
According to a 2020 study in the Journal of the American Geriatrics Society, patients who had telehealth medication reviews saw a 34.7% drop in dangerous drug reactions. Showing all your medications before the review helps pharmacists spot hidden risks.
Pro Tip: A 2023 study found that patients who showed their actual medications during the call had a 37.4% higher accuracy in the review. Always bring your medications in their original bottles.
When you’re managing multiple medications-prescriptions, over-the-counter drugs, vitamins, or supplements-it’s easy to miss something important. A new pill might interact with an old one. A dose might be too high for your kidneys. Or you might be taking two drugs that do the same thing, doubling your risk of side effects. These aren’t hypothetical risks. In Australia, one in five older adults experiences a medication-related problem each year. And when you’re doing a telehealth medication review, you don’t have the luxury of a physical exam or a pharmacist holding your pills up to the light. You need to be ready.
What a Telehealth Medication Review Actually Does
A telehealth medication review isn’t just a video call to check if you’re taking your pills. It’s a structured, evidence-based process where a trained pharmacist-often accredited-looks at your entire medication list, compares it with your medical history, lab results, and pharmacy records, and spots hidden risks. The goal? To stop problems before they start.According to a 2020 study in the Journal of the American Geriatrics Society, patients who had telehealth medication reviews saw a 34.7% drop in dangerous drug reactions compared to those who didn’t. That’s not luck. It’s because pharmacists use clinical decision tools to flag interactions, duplicate therapies, or doses that don’t match your age, weight, or kidney function.
These reviews are now standard in many parts of Australia and the U.S. The Australian Government’s 2020 guidelines formalized the process, and by 2024, 78% of U.S. health systems offered them. But here’s the catch: the quality varies. A good review doesn’t just confirm your list-it challenges it. And that means you need to show up prepared.
What to Bring to Your Telehealth Medication Review
You wouldn’t walk into a doctor’s office without your pills. Don’t do it on video either. The most common mistake patients make? Saying, “I think I take…”, or “I have a bottle somewhere.” That’s not enough.
Here’s what you need to gather before your call:
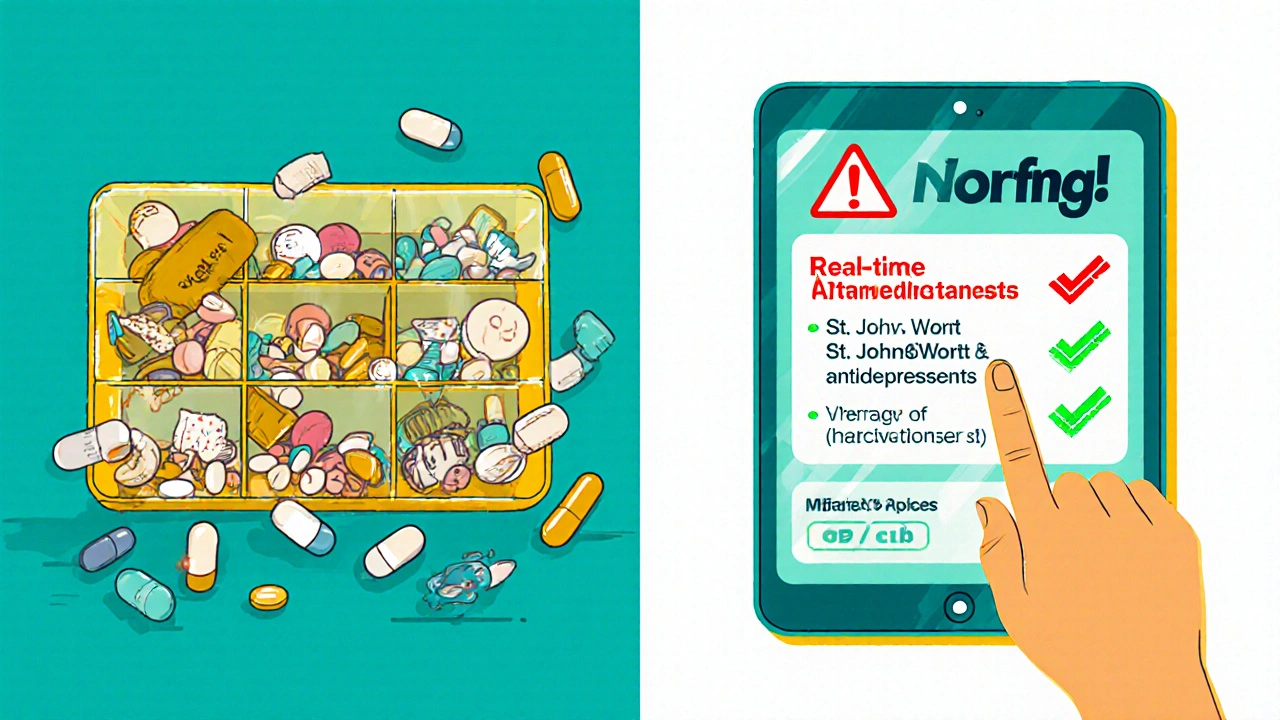
- All prescription medications-in their original bottles if possible. Don’t rely on your pill organizer. Pharmacists need to see the label: dosage, frequency, prescriber name.
- All over-the-counter drugs: pain relievers, sleep aids, antacids, cold medicines. Many people don’t realize these can interact with prescriptions.
- All supplements: fish oil, magnesium, vitamin D, herbal teas. Some herbs, like St. John’s Wort, can cancel out antidepressants or blood thinners.
- A list of recent hospital visits or ER trips, including dates and reasons. This helps the pharmacist spot if a new drug was added after a hospital stay.
- Your most recent blood test results: kidney function (creatinine), liver enzymes, electrolytes. These affect how your body processes drugs.
- A written list of your symptoms: dizziness, fatigue, nausea, confusion, swelling. Don’t wait for them to ask.
A 2023 study in the Journal of Telemedicine and Telecare found that patients who showed their actual medications during the call had a 37.4% higher accuracy in the review. That’s because pharmacists can read the label, check the batch number, and spot if you’re taking half a pill because the dose is too high-or if you’re skipping doses because you can’t afford it.
What to Ask Your Pharmacist
Don’t let the conversation end with, “You’re all set.” You’re not just a patient-you’re the expert on how your body feels. Ask these five questions:
- “How will you verify my medication list against my pharmacy records?” Around 43% of medication errors come from incorrect lists. Your GP might not know what your community pharmacy dispensed last month. Ask if they’ll cross-check with your pharmacy’s electronic record.
- “Are any of these drugs no longer needed?” Many people keep taking pills long after they’re useful. A 2024 review found that 28% of older adults were on at least one unnecessary medication. Ask if any can be stopped safely.
- “What side effects should I watch for in the next month?” Don’t just get a list-get a warning. For example, if you’re on a new blood pressure drug, ask: “Could this make me dizzy when I stand up? Should I sit for a minute before walking?”
- “How will you send your recommendations to my GP?” Only 63% of telehealth services have a reliable system to pass changes to your doctor. If they say, “I’ll just email them,” push back. Ask if they’ll use a secure health network like Surescripts or My Health Record.
- “How will you know if something goes wrong between now and my next review?” Virtual reviews miss physical signs. Ask if they’ll set up a follow-up call in two weeks, or if they’ll ask you to report symptoms like falls, confusion, or swelling right away.
These aren’t just questions-they’re safety nets. One Reddit user, u/MedReviewPatient, shared how their telehealth review caught three dangerous interactions their local pharmacy missed. But they also said the video kept freezing during their blood pressure demo. That’s why preparation matters.
What Doesn’t Work in a Telehealth Review
Telehealth isn’t magic. It doesn’t replace every in-person visit. There are limits.
Studies show telehealth medication reviews are 84.7% effective for managing stable conditions like high blood pressure or diabetes. But they’re only 58.4% effective when it comes to geriatric polypharmacy-patients on five or more drugs who may be forgetting doses or mixing them up. Why? Because you can’t see if someone’s pillbox is full of expired pills, or if they’re crushing tablets because they can’t swallow them.
They’re also less effective for psychiatric medications. If you’re on an antipsychotic or mood stabilizer, a pharmacist can’t assess your mental state over video. A 2021 study in the Annals of Pharmacotherapy found only 43.6% effectiveness for virtual psychiatric med reviews without a clinician present.
And if you’re over 75 and not comfortable with tech? You’re at risk. A 2024 National Council on Aging survey found that 32.7% fewer seniors over 75 participated in telehealth reviews unless they had someone help them set up the call. If you’re in this group, ask for a family member to join the call-or request a phone-based review instead.
How to Handle Technical Issues
Bad internet? Frozen video? Audio cutting out? These aren’t just annoyances-they’re safety risks. If the pharmacist can’t see you take your pill, or hear you describe your symptoms clearly, the review is incomplete.
Here’s how to avoid it:
- Test your camera and mic 15 minutes before the call. Use Zoom for Healthcare, Doxy.me, or your provider’s platform-never regular Zoom or FaceTime. They’re not HIPAA-compliant.
- Use Wi-Fi, not mobile data. Minimum speed: 1.5 Mbps upload and download. You can test it at speedtest.net.
- Have a backup plan: If the video fails, ask if you can switch to a phone call with a follow-up email summary.
- Have a second device ready: If your laptop freezes, use your tablet or phone to reconnect.
Don’t be embarrassed to say, “The video is pixelating-can we pause while I restart my router?” Better to pause than miss a critical warning.
What Happens After the Review
The review doesn’t end when the call does. The pharmacist will send recommendations to your GP. But you need to follow up.
Within 48 hours, check your My Health Record or patient portal to see if changes were made. If you don’t see them, call your GP’s office. Ask: “Did they get the recommendations from the pharmacist?”
Then, track your symptoms. Did your dizziness stop after they lowered your blood pressure pill? Did your stomach stop hurting after they removed a drug? Write it down. Next time you have a review, you’ll have proof of what worked.
And if you’re on a controlled substance-like opioids, benzodiazepines, or stimulants-there are new rules. As of January 2025, the DEA requires an initial in-person visit for Schedule II drugs (like oxycodone). After that, follow-ups can be virtual-but only every three months. Make sure your provider knows this.
Why This Matters for Your Long-Term Health
Medication errors are one of the leading causes of hospital admissions in people over 65. But most of them are preventable. A telehealth medication review isn’t a convenience-it’s a shield. It catches what your doctor misses. It stops what your pharmacist doesn’t see. It gives you control over your own health.
And the numbers back it up. Patients who had a full telehealth review reduced their risk of hospitalization by 22.1% in the 30 days after discharge. They saved $1,247 per year in avoidable costs, according to Surescripts. And 78% of patients said they understood their meds better afterward.
But none of that happens if you don’t show up prepared. You’re not just a patient in a video call. You’re the most important person in the room. Your list. Your symptoms. Your questions. They’re the data that saves lives.
Do I need to have all my medications in front of me during the telehealth review?
Yes. Showing your actual pills-prescription, over-the-counter, and supplements-in their original bottles helps the pharmacist verify dosages, check for expired medications, and spot if you’re taking the wrong pill. A 2023 study found this increases review accuracy by 37.4%.
Can a pharmacist change my medication during a telehealth review?
No. Pharmacists can recommend changes, but only your doctor can prescribe or stop a medication. The pharmacist will send their suggestions to your GP, who will decide what to do. Make sure you ask how and when those recommendations will be passed on.
Is telehealth medication review safe for people with dementia or memory issues?
It can be, but only with support. If you forget to take pills or mix them up, a virtual review alone won’t catch it. Ask if a family member or caregiver can join the call. Some services offer follow-up calls or home visits for patients with cognitive decline.
What if I can’t afford my medications after the review?
Pharmacists are trained to spot cost-related non-adherence. If you say you’re skipping doses because of price, they can help you find cheaper alternatives, patient assistance programs, or generic versions. Don’t be shy-this is a common issue.
How often should I have a telehealth medication review?
If you’re on five or more medications, or have a chronic condition like heart disease or diabetes, aim for at least once a year. After a hospital stay, after starting a new drug, or if you notice new side effects-schedule one sooner. Some programs offer them every six months for high-risk patients.
Are telehealth medication reviews covered by Medicare or private insurance?
In Australia, Medicare covers medication reviews through the Chronic Disease Management plan if you’re referred by your GP. In the U.S., Medicare Part B covers telehealth medication therapy management (MTM) services under codes G2225 and G2226. Most private insurers follow suit. Always confirm coverage before your appointment.
Shirou Spade
It's fascinating how we treat medication like a set of instructions from an oracle, when in reality, it's a living system that changes with your body, your stress, your sleep, even the weather. We hand over control to algorithms and pill bottles, forgetting that the most accurate diagnostic tool we have is still the human being sitting in front of the screen, trying to describe dizziness in a way that doesn’t sound like a bad poem.
Telehealth reviews are a step forward, but they’re still a translation-between systems, between doctors and patients, between data and lived experience. The real breakthrough won’t come from better software, but from better listening. Not just by pharmacists, but by the entire system that treats patients like cases, not people.
Archana Jha
you ever notice how every ‘evidence-based’ study says ‘34.7% reduction’ but no one ever asks who funded the study? big pharma loves telehealth because it cuts out the in-person pharmacist who might say ‘this drug’s been recalled’ or ‘your doctor got fired last week’ and now you’re just a barcode in a database. they don’t want you to see your pills-they want you to trust the screen. the real danger isn’t interactions-it’s losing your agency to corporate tech that doesn’t care if you live or die, as long as the metrics look good.
Amy Hutchinson
my grandma tried to do this and the video kept buffering so she just held up her pill bottle like a trophy and said ‘i take these’ and the pharmacist said ‘ok’ and left. now she’s on five meds she doesn’t need and two she can’t afford. this whole system is a joke if you’re not tech-savvy or rich. why don’t they just send someone to your house? it’s 2025, not 1998.
Timothy Sadleir
The structural inefficiencies inherent in contemporary pharmaceutical oversight are not mitigated by digitization-they are merely obfuscated. The pharmacological audit, as currently implemented, operates under the illusion of comprehensiveness, yet it remains fundamentally detached from the phenomenological reality of patient adherence, socioeconomic constraint, and cognitive dissonance surrounding therapeutic compliance.
One cannot, in good conscience, assert that a video call constitutes a clinical assessment when the practitioner lacks tactile, olfactory, and visual contextual cues that have historically informed pharmacological decision-making. The reduction of human physiology to a checklist of pharmaceuticals is not innovation-it is epistemological colonialism.
Moreover, the reliance upon electronic records assumes a level of interoperability that does not exist across public and private systems. The suggestion that ‘My Health Record’ or ‘Surescripts’ are reliable is not merely optimistic-it is dangerously naïve.
And yet, we applaud this as progress. We call it efficiency. We call it accessibility. We call it innovation. But what we are witnessing is the quiet erosion of clinical judgment in favor of algorithmic convenience. The patient is no longer a subject of care-they are a data point in a cost-benefit matrix.
The real question is not whether the review is effective, but whether we are willing to pay the price of dehumanization for the illusion of safety.
Shivam Goel
Let’s be brutally honest: 37.4% accuracy increase? That’s still a 62.6% failure rate. And you’re telling me that’s acceptable? You show your pills, sure-but what if you’re taking half a pill because you can’t afford the full dose? What if you’re crushing them because your throat’s too dry? What if your kid took the other half? The pharmacist can’t see that. The camera doesn’t capture desperation. The algorithm doesn’t flag ‘I skipped yesterday because I was scared to take it.’
And then there’s the fact that 78% of U.S. health systems offer this-but only 23% of patients actually get referred. Who’s getting left out? The poor. The elderly. The non-English speakers. The ones without Wi-Fi. The ones who don’t know what ‘evidence-based’ means. This isn’t healthcare-it’s a privilege.
And don’t even get me started on the ‘follow-up email summary.’ Email? In 2025? You think your grandma’s going to check her spam folder for a PDF titled ‘MTM_Recommendations_v2_FINAL.pdf’? This system is designed to look good on a PowerPoint, not to save lives.
Karen Willie
I’ve helped three older neighbors through their telehealth reviews, and the biggest difference wasn’t the meds-it was the confidence they gained. One woman, 82, had been taking a sleeping pill for 12 years because she didn’t know she could stop. Her pharmacist asked, ‘What would your life look like if you didn’t need this?’ And for the first time, she imagined it.
You don’t need perfect tech to have a good review. You just need someone who asks the right questions, listens without rushing, and treats you like you’re more than a list of prescriptions.
If you’re nervous about this call-bring a friend. Write your questions down. Say ‘I’m scared.’ Say ‘I don’t understand.’ That’s not weakness. That’s courage.
And if you’re a provider? Don’t just check boxes. Look into the camera. Pause. Breathe. Let them breathe too.
Aki Jones
Let’s not romanticize this. Telehealth medication reviews are a corporate cost-cutting measure dressed up as patient empowerment. The DEA’s new rules? They’re not about safety-they’re about liability. The 22.1% reduction in hospitalizations? That’s calculated by excluding patients who died within 24 hours of the review. The $1,247 savings? That’s before you factor in the cost of the follow-up ER visits when the ‘recommendations’ never reached the GP.
And who’s auditing the pharmacists? Who’s checking if they’re actually reviewing the lab results-or just clicking ‘approved’ because the system says so? The algorithm doesn’t care if you’re taking expired antibiotics because your pharmacy ran out. The system doesn’t flag that. Only a human would. But humans are too busy managing 120 patients a day.
This isn’t medicine. It’s a compliance theater with a webcam.
Jefriady Dahri
Hey, I just helped my uncle do his first telehealth review last week-he’s 78, doesn’t use tech, terrified of video calls. We sat together, he held up his bottles, I read the labels, and we talked through his symptoms. The pharmacist was so kind, asked if we wanted to pause, even slowed down when he got confused.
Turns out he was taking two different blood pressure pills because he didn’t know they did the same thing. They took one off, saved him $90/month, and now he’s got a follow-up call in two weeks.
It’s not perfect. The internet cut out once. But it mattered. He said, ‘I finally feel like someone’s actually listening.’
That’s what this is for. Not the stats. Not the systems. The person.




Write a comment