When you pick up a generic pill at the pharmacy, you might wonder: is this really the same as the brand-name version you used to take? The answer isn’t as simple as it seems - and one number keeps popping up in conversations: 80-125%. But here’s the thing most people get wrong. That number doesn’t mean your generic drug has 25% less or 25% more active ingredient. It’s not about how much drug is in the tablet. It’s about how your body absorbs it.
What the 80-125% Rule Actually Measures
The 80-125% rule is a bioequivalence standard used by the FDA and other global regulators to prove that a generic drug works the same way as the brand-name version. It’s not a tolerance for how much active ingredient is in the pill - it’s a measure of how quickly and completely your body absorbs the drug into your bloodstream.
Two key numbers are tracked: AUC (area under the curve) and Cmax (peak concentration). AUC tells you how much of the drug your body is exposed to over time - the total amount absorbed. Cmax tells you how fast it gets there - the peak level in your blood. For a generic to be approved, the 90% confidence interval of the ratio between the generic and brand drug’s AUC and Cmax must fall entirely within 80% to 125%.
That’s not the same as saying the generic can be 20% weaker or 25% stronger. It’s a statistical boundary that accounts for normal variation between people, testing conditions, and even lab measurements. In practice, most approved generics have absorption rates within 90-110% of the brand. A 2012 FDA analysis of over 2,000 studies found 98% of generics fell within that tighter range.
Why 80-125%? Not 80-120%
You might wonder why the range isn’t symmetrical - why 125% instead of 120%? It comes down to math. Drug absorption data doesn’t follow a straight line; it follows a log-normal distribution. That means differences are measured on a logarithmic scale. When you take the natural log of 0.80, you get -0.223. To keep the scale balanced, the upper limit becomes exp(0.223), which equals 1.25 - or 125%. This isn’t arbitrary. It’s the mathematically correct way to compare variability in absorption rates.
If regulators used a simple ±20% rule (80-120%), it would unfairly penalize drugs with naturally high variability in how they’re absorbed. The 80-125% range, paired with a 90% confidence interval, ensures that even if a generic’s average absorption is slightly off, the real difference between it and the brand is almost certainly less than 10%.
Real-World Performance: Do Generics Work the Same?
Here’s what matters most: do patients actually get the same results? Yes. A 2016 study in JAMA Internal Medicine looked at over 2 million patients taking generic versions of cardiovascular drugs. There was no difference in heart attacks, strokes, or hospitalizations between those on brand and generic versions.
The FDA’s Sentinel Initiative, which tracks 200 million patient records, found no significant rise in adverse events for 94% of generic drugs between 2015 and 2020. For drugs like statins, blood pressure meds, and antidepressants, the outcomes are identical.
Even more telling: the average difference in absorption between brand and generic drugs is just 3.5%, according to FDA data. That’s less than the natural variation you’d see if the same person took the same brand-name drug twice - one morning on an empty stomach, another after a big meal.
Where the Rule Gets Tricky: Narrow Therapeutic Index Drugs
Not all drugs are created equal. For drugs with a narrow therapeutic index - where even small changes in blood levels can cause serious side effects or make the drug ineffective - the 80-125% rule isn’t enough. That’s why the FDA applies tighter standards for drugs like warfarin (a blood thinner), levothyroxine (for thyroid conditions), and some anti-seizure medications.
For these, the acceptable range is 90-111%. This means the generic must be absorbed almost identically to the brand. The FDA requires more rigorous testing, often with more participants and repeated dosing, to make sure there’s no risk.
And here’s the key: pharmacists know this. If you’re prescribed one of these drugs, your pharmacist will usually check whether the generic you’re getting is approved under the stricter standard. You don’t need to ask - they’re trained to spot it.
Why the Myth Persists
Despite all the data, the myth that generics can be “25% weaker” still spreads. Pharmacy students on forums like Student Doctor Network have posted threads with hundreds of comments misunderstanding the rule. Reddit users share stories of anxiety over switching to generics. One pharmacist reported that 78% of patients ask about the 80-125% rule at least once a week.
Why does this myth stick? Because it sounds plausible. “If it’s cheaper, it must be less,” is a natural assumption. But the truth is, generics are made with the same active ingredient, same dosage form, and same strict manufacturing standards. The only differences are in fillers, coatings, or packaging - none of which affect how the drug works.
The FDA’s #GenericsWork campaign was launched to tackle this exact issue. After 1.2 million views on social media, patient confidence rose. Surveys show that once people understand the science, their fears fade.
How Bioequivalence Studies Work
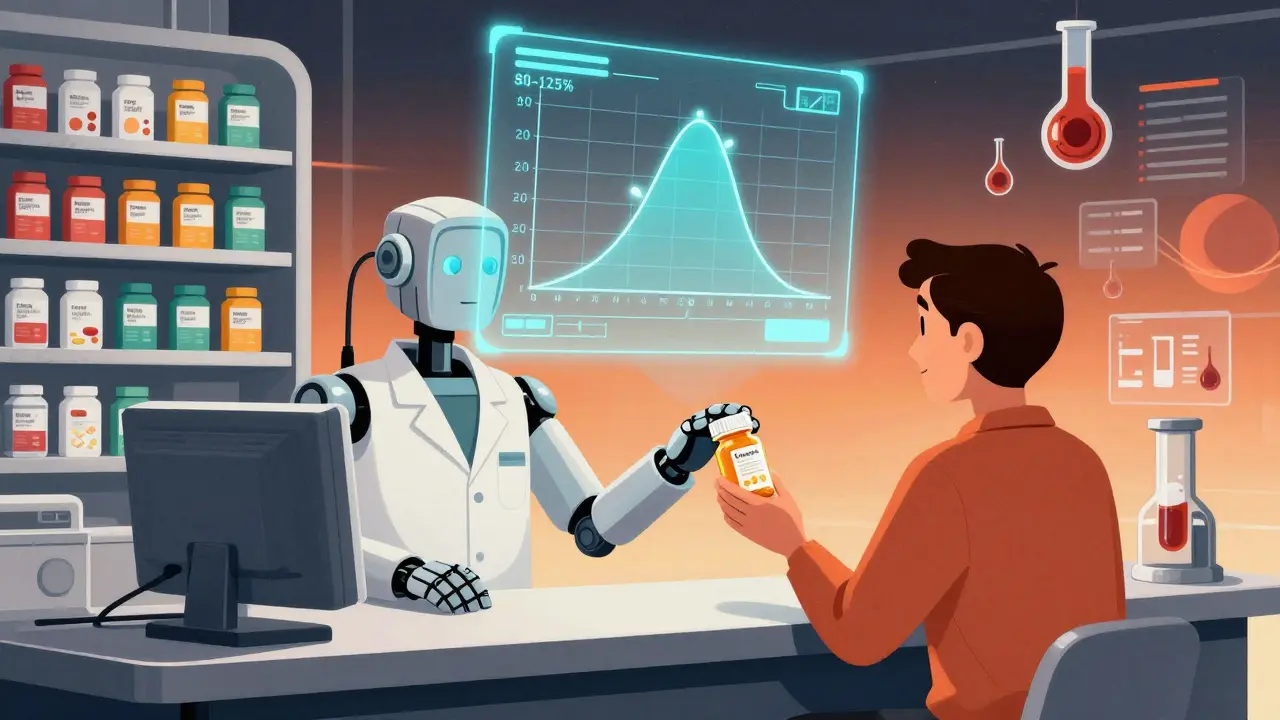
Before a generic hits the shelf, it goes through a clinical study. Typically, 24 to 36 healthy volunteers take both the brand and generic versions in a crossover design - meaning half take the brand first, then the generic; the other half do the reverse. Blood samples are taken every 15 to 30 minutes over 72 hours to map out how the drug enters and leaves the bloodstream.
The lab must measure concentrations with precision - no more than 15% variation between tests. The data is log-transformed, the 90% confidence interval is calculated, and only if it fits entirely within 80-125% does the FDA approve the generic.
It’s not easy. In 2022, 32% of generic applications were rejected or delayed because the bioequivalence data didn’t meet the standard. That’s not because companies are cutting corners - it’s because the bar is high, and the math doesn’t lie.
What This Means for You
If you’re taking a generic drug, you’re getting the same medicine as the brand - just at a fraction of the cost. Generics now make up 90% of all prescriptions in the U.S., saving the healthcare system over $370 billion in 2021 alone. That’s not a coincidence. It’s proof that the system works.
For most people, switching from brand to generic is safe, effective, and smart. If you’re on a narrow therapeutic index drug, your doctor or pharmacist will let you know if extra care is needed. But for the vast majority - antibiotics, blood pressure pills, cholesterol meds, pain relievers - there’s no reason to worry.
And if you’re still unsure? Ask your pharmacist. They’re trained to explain the science. Most will show you the FDA’s data. They’ve seen the studies. They’ve watched patients thrive on generics for years.
What’s Next for Generic Drugs?
The FDA is working on new tools to handle complex generics - things like inhalers, topical creams, and injectables where absorption can’t be measured easily through blood tests. By 2025, they plan to use computer models to predict how these drugs behave in the body, reducing the need for large human trials.
But the core rule - 80-125% with a 90% confidence interval - isn’t going anywhere. It’s been tested for over 30 years. It’s been upheld in court. And every day, millions of people rely on it without even knowing it.
So next time you see a generic on your prescription, remember: it’s not a compromise. It’s science.
Does the 80-125% rule mean generic drugs have less active ingredient?
No. The 80-125% rule does not refer to the amount of active ingredient in the pill. It measures how much of that ingredient your body absorbs into the bloodstream. Generic drugs must contain the exact same amount of active ingredient as the brand-name version. The rule ensures that absorption rates are similar enough to produce the same therapeutic effect.
Are generic drugs as safe as brand-name drugs?
Yes. Generic drugs must meet the same strict manufacturing standards as brand-name drugs. The FDA inspects generic manufacturing facilities with the same frequency and rigor. Studies tracking millions of patients show no difference in safety or effectiveness between brand and generic versions of most medications.
Why do some people say generics don’t work as well?
This usually comes from misunderstanding the 80-125% rule or from placebo effects. Some patients feel better when they believe they’re taking the more expensive brand. In reality, studies show no difference in outcomes. For drugs with narrow therapeutic indexes, like warfarin or levothyroxine, stricter standards apply, and pharmacists are trained to monitor these cases closely.
Can I switch between different generic brands?
Yes. All approved generics for the same drug must meet the same bioequivalence standards. Switching between different generic manufacturers is safe for most drugs. However, if you’re on a narrow therapeutic index drug, your doctor may recommend sticking with one brand to avoid any potential variability, even if it’s minimal.
Do generic drugs take longer to work?
Not if they’re bioequivalent. The Cmax measurement ensures that the peak concentration in your blood happens at a similar time as the brand-name drug. Most generics reach peak levels within minutes of each other. If you notice a delay, it could be due to food, stomach emptying, or other personal factors - not the drug itself.
matthew martin
Man, I used to freak out switching to generics until I dug into the bioequivalence stuff. Turns out the 80-125% thing isn’t a loophole - it’s a mathematically elegant way to account for real human variation. Like, your body absorbs caffeine differently on a full stomach vs. empty, right? Same deal here. The FDA’s not letting junk through - they’re just being smart about biology.
jonathan soba
Still think it’s BS. My cousin took a generic antidepressant and felt like a zombie for three weeks. Switched back to brand - boom, normal again. Stats don’t care about real people.
matthew martin
That’s not the rule failing - that’s individual variability. Maybe your cousin metabolizes drugs differently, or had a bad batch. The FDA’s data shows 98% of generics are within 90-110%. One anecdote doesn’t invalidate a system tested on millions. Also, placebo effect is wild - people *feel* worse on generics because they expect to.




Write a comment