
Sleep Apnea & Glaucoma Risk Calculator
Risk Assessment
Answer the following questions to assess your risk of developing glaucoma due to sleep apnea.
Your Risk Assessment
Key Takeaways
- Obstructive sleep apnea (OSA) can raise eye pressure, increasing glaucoma risk.
- Both conditions share vascular and pressure‑related mechanisms.
- Regular eye exams and sleep studies are crucial for early detection.
- Effective OSA treatment, especially CPAP, may slow glaucoma progression.
- Lifestyle changes-weight control, sleep hygiene, and regular exercise-help manage both disorders.
What Is Sleep Apnea?
When breathing repeatedly stops or drops during sleep, the condition is called sleep apnea a disorder where airway blockage causes brief pauses in breathing, leading to reduced oxygen levels and fragmented sleep. The most common form, obstructive sleep apnea (OSA), occurs when throat muscles relax too much, collapsing the airway.
Key signs include loud snoring, morning headaches, daytime sleepiness, and a choking sensation at night. If untreated, OSA can strain the heart, raise blood pressure, and trigger metabolic problems.
What Is Glaucoma?
Glaucoma a group of eye diseases characterized by damage to the optic nerve, often linked to elevated intraocular pressure (IOP) is the second leading cause of blindness worldwide. The most familiar type, primary open‑angle glaucoma, develops slowly and may have no symptoms until vision loss occurs.Typical warning signs are peripheral vision loss, tunnel‑vision effect, and occasional eye pain. Early detection through routine eye scans can preserve sight.
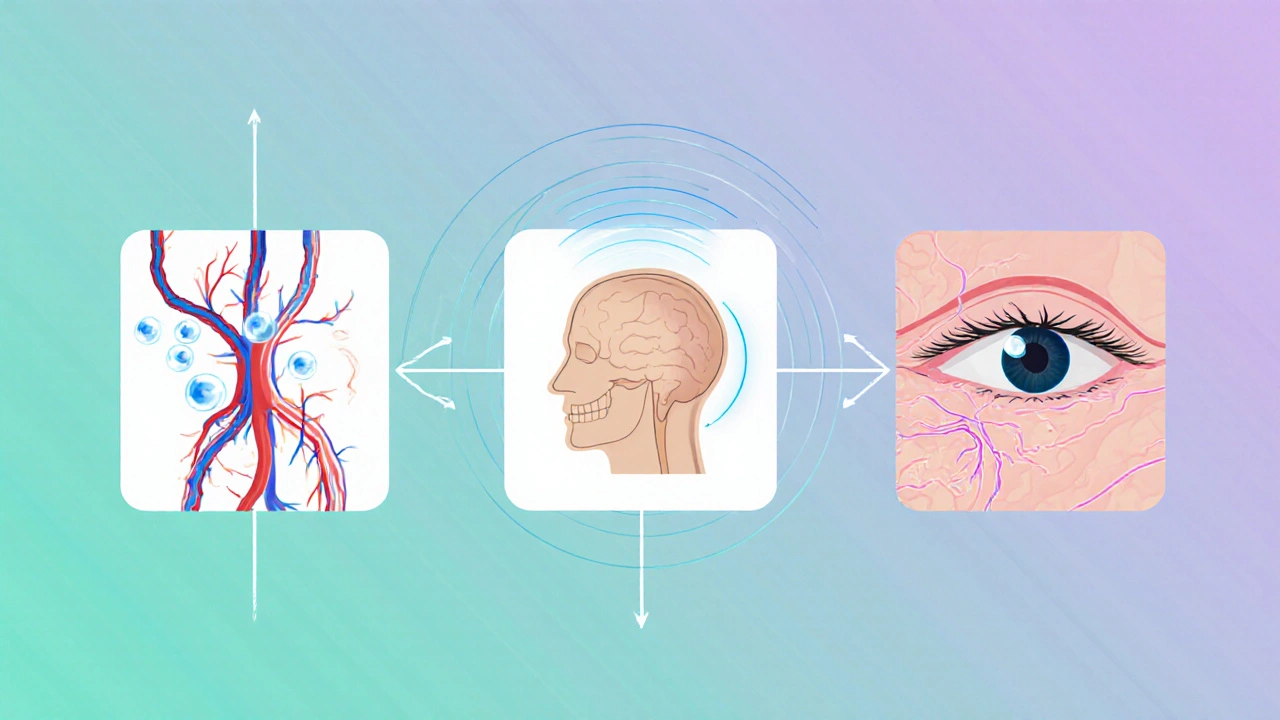
How Do Sleep Apnea and Glaucoma Connect?
Researchers have identified three main pathways linking OSA to glaucoma:
- Fluctuating oxygen levels: Repeated drops in blood oxygen during apnea episodes can stress the optic nerve, similar to how a power surge damages an electrical circuit.
- Increased intracranial pressure: The effort to breathe against a blocked airway raises pressure in the head, which can push fluid into the eye and temporarily spike intraocular pressure.
- Vascular dysregulation: OSA often co‑exists with hypertension and diabetes, conditions that impair blood flow to the retina and optic nerve.
One longitudinal study of 7,200 adults showed that OSA sufferers had a 1.8‑fold higher odds of developing glaucoma over ten years, even after adjusting for age, smoking, and systemic disease.
Who Is Most at Risk?
While anyone can develop either condition, certain groups face higher combined risk:
- Adults over 50 with a body‑mass index (BMI) above 30.
- People with a family history of glaucoma or OSA.
- Individuals of African or Asian descent, who statistically show higher glaucoma prevalence.
- Patients with hypertension, type 2 diabetes, or cardiovascular disease.
For these groups, a proactive screening strategy is especially worthwhile.
Symptoms to Watch For
Sleep‑related clues often appear before eye‑related ones. If you notice chronic fatigue, unexplained weight gain, or a dry mouth each morning, consider a sleep study.
Eye‑related clues may include:
- Gradual loss of side‑vision (often unnoticed until advanced).
- Difficulty adjusting to low light.
- Eye redness or occasional mild pain, especially after waking.
Because early glaucoma can be silent, regular eye checks remain the only reliable way to catch it.
Diagnosis and Screening
Two separate but complementary tests are essential:
- Polysomnography (sleep study): Conducted overnight in a lab, this test records breathing patterns, oxygen saturation, and brain activity. The gold‑standard for confirming OSA severity.
- Comprehensive eye exam: An ophthalmologist measures intraocular pressure with a tonometer, evaluates the optic nerve via optical coherence tomography (OCT), and maps peripheral vision with a Humphrey visual field test.
When both tests reveal moderate to severe OSA and elevated IOP, clinicians often refer patients to a multidisciplinary team-sleep specialists and eye doctors-to coordinate care.
Managing the Risk: Treatment Options
Addressing OSA can directly influence glaucoma outcomes. The primary OSA therapy, CPAP continuous positive airway pressure, a machine that delivers steady air flow to keep the airway open during sleep, has been shown to lower nightly spikes in intraocular pressure by up to 15% in several small trials.
Glaucoma treatment still follows standard protocols:
- Topical eye drops (e.g., prostaglandin analogues) to lower IOP.
- Laser trabeculoplasty for opening drainage pathways.
- Surgical options like minimally invasive glaucoma surgery (MIGS) when medication fails.
Coordinating these approaches means:
- Ensuring CPAP pressure settings do not inadvertently raise ocular pressure-a rare but documented issue.
- Scheduling eye exams at least annually for OSA patients, or more often if they already have glaucoma.

Lifestyle Changes That Help Both Conditions
Simple daily habits can lower the odds of both OSA and glaucoma:
- Weight management: Losing 5-10% of body weight can reduce apnea events by 30% on average.
- Sleep hygiene: Keeping a consistent bedtime, elevating the head of the bed by 4 inches, and avoiding alcohol before sleep improve airway tone.
- Regular exercise: Aerobic activity boosts circulation to the optic nerve and improves overall respiratory function.
- Eye protection: Wearing sunglasses reduces UV‑induced ocular stress, which can compound glaucoma risk.
Prevalence Comparison
| Population | Glaucoma Cases (%) | Study Year |
|---|---|---|
| OSA diagnosed (moderate‑severe) | 7.2 | 2022 |
| OSA negative (matched controls) | 4.1 | 2022 |
| General adult population | 3.5 | 2020 |
The data make it clear: people with untreated OSA face a noticeably higher chance of developing glaucoma.
When to Seek Professional Help
If you notice any combination of the following, schedule appointments promptly:
- Persistent loud snoring with observed breathing pauses.
- Morning headaches or excessive daytime sleepiness.
- Noticeable loss of side vision, especially in low‑light environments.
- Diagnosed OSA but no recent eye exam in the past year.
Early intervention can preserve both sleep quality and sight.
Bottom Line
The connection between sleep apnea and glaucoma isn’t just a coincidence; it’s a physiological link that magnifies eye‑health risk. By combining regular sleep assessments, diligent eye checks, targeted treatments like CPAP, and lifestyle tweaks, you can dramatically lower your odds of vision loss.
Frequently Asked Questions
Can treating sleep apnea reverse glaucoma?
Treating OSA can stabilize intraocular pressure and may slow glaucoma progression, but it rarely reverses existing optic‑nerve damage. Early treatment combined with standard glaucoma therapy offers the best chance to protect remaining vision.
Is CPAP safe for people with glaucoma?
CPAP is generally safe and can even lower nightly eye‑pressure spikes. However, some patients experience mask‑related eye irritation; a good fit and regular cleaning prevent this.
How often should I get an eye exam if I have OSA?
At minimum, an annual dilated eye exam is advised. If you already have glaucoma, follow your ophthalmologist’s schedule, which may be every 3‑6 months.
Do lifestyle changes impact both conditions?
Yes. Weight loss, regular exercise, and good sleep hygiene can reduce apnea severity and improve blood flow to the optic nerve, lowering overall glaucoma risk.
Are there any medications that affect both sleep apnea and glaucoma?
Certain sedatives can worsen OSA by relaxing airway muscles, while some glaucoma eye drops (like beta‑blockers) may lower heart rate, affecting sleep quality. Always discuss all meds with both your sleep specialist and ophthalmologist.
Preeti Sharma
While most readers may accept the link between sleep apnea and glaucoma at face value, consider the broader physiological cascade that intertwines vascular dysregulation and optic nerve perfusion. The intermittent hypoxia of apnea episodes initiates systemic inflammation, which can subtly compromise ocular blood flow over time. Thus, the risk calculator is a useful heuristic, yet it abstracts a complex neurovascular dialogue. One should interpret its output as a prompt for comprehensive ophthalmic evaluation rather than a definitive verdict.
Ted G
What they don't tell you is that these "risk calculators" are part of a larger surveillance network feeding data to shadowy health conglomerates. Every click, every symptom you tick off, fuels algorithms that push pharmaceutical solutions directly into your inbox. The true danger lies not in glaucoma itself, but in the commodification of your vulnerability. Stay alert, question the motives behind every health app you trust.
Miriam Bresticker
Ah, the entanglement of nocturnal breathlessness and optic pressure is like a cosmic dance of dis‑ease 🤔. If you think the questionnaire is merely a simple checklist, you miss the subtle rhythm of autonomic imbalance 🌙. The body, in its nocturnal silence, whispers hints that only a keen eye can translate into preventive action. 🧐
Claire Willett
Targeted screening using this tool can streamline referrals and allocate resources efficiently. Early detection remains the cornerstone of preserving visual fields. Integrate it into routine assessments for patients with documented apnea.
olivia guerrero
Absolutely love how this brings awareness!! 🌟 It's a fantastic step forward, and everyone should give it a try!!! 😊
Dominique Jacobs
Alright folks, this is exactly the kind of proactive health hack we need! Plug in those answers, see where you stand, and then smash that follow‑up appointment with your eye doc. No more waiting for symptoms to creep up – beat the system at its own game!
Claire Kondash
In the grand tapestry of human physiology, the night‑time cessation of breath is not merely a nuisance, but a profound signal that reverberates through the ocular vasculature.
Every apneic episode delivers a cascade of hypoxic stress, prompting endothelial dysfunction that subtly erodes the delicate autoregulatory mechanisms safeguarding the optic nerve.
This erosion, over months and years, translates into a silent elevation of intra‑ocular pressure, a risk factor that lurks unnoticed until vision wanes.
Thus, the calculator presented here serves as a modest lantern, illuminating a path that might otherwise be shrouded in darkness.
Yet, the true wisdom lies in understanding that such tools are adjuncts, not replacements, for comprehensive clinical assessment.
When you answer "yes" to snoring, you flag a mechanical obstruction that may demand CPAP therapy, which itself has been shown to mitigate nocturnal blood pressure spikes.
Recognizing daytime sleepiness reinforces the narrative that systemic fatigue mirrors ocular strain, urging clinicians to probe deeper into retinal nerve fiber layer thickness.
The presence of hypertension compounds the story, as vascular rigidity amplifies pressure fluctuations within the optic disc.
Obesity, the metabolic heavyweight, contributes to inflammatory mediators that further destabilize ocular homeostasis.
Family history, the genetic echo, reminds us that susceptibility can be inherited, making vigilant monitoring paramount.
Collectively, these variables coalesce into a risk score that, while not definitive, offers a quantifiable glimpse into potential disease trajectory.
Importantly, the score should catalyze action – a referral to an ophthalmologist for optic nerve imaging, visual field testing, and perhaps a discussion about nocturnal CPAP adherence.
Do not let the numbers lull you into complacency; they are prompts for dialogue, not verdicts.
Consider also lifestyle interventions – weight management, blood pressure control, and sleep hygiene – as integral components of a holistic strategy.
Remember, the eyes are windows to systemic health, and what transpires in the darkness of night can shape the clarity of your daylight vision.
Embrace this tool as a stepping stone, and let it guide you toward informed, proactive ocular care.
🌙👁️
Matt Tait
If you think ticking boxes on a website is enough, you’re living in a delusional bubble. The calculator oversimplifies a multi‑factorial disease into a five‑question quiz, which is frankly lazy. Real risk assessment demands detailed sleep studies and tonometry, not this gimmick.
Benton Myers
Cool tool, thanks.
jennifer jackson
Glad this is out there, it's really helpful!
Brenda Martinez
Let me lay it out plainly: the correlation between obstructive sleep apnea and glaucomatous optic neuropathy is well‑documented in peer‑reviewed literature, and the pathophysiology hinges on intermittent hypoxia, oxidative stress, and vascular dysregulation. Ignoring these findings in clinical practice is not just negligent-it’s a disservice to patients who could benefit from early intervention. The risk calculator, while simplistic, is a stepping stone toward that vigilance. If you’re still skeptical, dive into the recent meta‑analyses; the data speak louder than any anecdote.
Marlene Schanz
For anyone looking to use this, make sure to follow up with a comprehensive eye exam. The calculator can flag risk, but only an ophthalmologist can confirm early glaucomatous changes. Also, consider discussing CPAP adherence with your sleep specialist to potentially lower overall risk.
Matthew Ulvik
Hey all, just a heads up – if you’ve got sleep apnea, it’s worth getting your eyes checked even if you feel fine. A quick chat with your doctor can set you on the right path.


Write a comment