
Dealing with a stubborn rash that won’t clear up? You’ve probably heard of Lotrisone, the combo of a steroid and an antifungal. But is it really the best option, or are there other creams that might work better for your skin type, infection type, or lifestyle? This guide breaks down what Lotrisone does, how it stacks up against popular alternatives, and how to pick the right product for you.
Key Takeaways
- Lotrisone mixes betamethasone (a potent steroid) with clotrimazole (a broad‑spectrum antifungal).
- It’s excellent for inflamed, itchy fungal infections but can thin skin if used too long.
- Hydrocortisone + Miconazole, Ketoconazole, Terbinafine, and Nystatin are common non‑prescription or prescription rivals.
- Choose based on infection type (tinea vs. candida), skin sensitivity, and how quickly you need relief.
- Always follow a doctor’s advice for prolonged or facial use.
What Is Lotrisone?
Lotrisone is a topical cream that combines betamethasone dipropionate, a high‑potency corticosteroid, with clotrimazole, an azole‑class antifungal. It was first approved by the FDA in 1995 and is marketed for mixed fungal‑and‑inflammatory skin conditions such as athlete’s foot, jock itch, and certain types of dermatitis.
How the Two Ingredients Work Together
Betamethasone reduces redness, swelling, and itching by suppressing the local immune response. It’s about 20‑30 times stronger than hydrocortisone, making it suitable for short‑term flare‑ups.
Clotrimazole disrupts the fungal cell membrane by inhibiting ergosterol synthesis, effectively stopping the growth of dermatophytes (like Trichophyton) and yeasts (like Candida).
The steroid calms the skin’s reaction while the antifungal attacks the pathogen, delivering faster symptom relief than either component alone.
When to Use Lotrisone
- Diagnosed fungal infection that’s also inflamed (e.g., tinea corporis with intense itching).
- Short‑term treatment: typically 2‑4 weeks, not more than 6 weeks without medical supervision.
- Areas with thick skin (feet, groin) where higher steroid potency is tolerated.
Do not apply to the face, intertriginous zones (skin folds) for extended periods, or on broken skin without a doctor’s OK, as the steroid can increase absorption and cause systemic effects.
Top Alternatives to Lotrisone
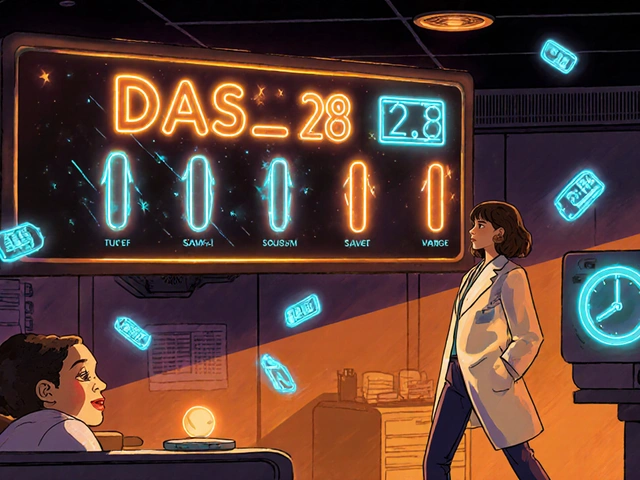
| Product | Active Ingredients | Steroid Strength | Antifungal Spectrum | Typical Use‑Duration | Prescription Needed? |
|---|---|---|---|---|---|
| Lotrisone | Betamethasone 0.1 % + Clotrimazole 1 % | High (potent) | Broad (dermatophytes, Candida) | 2‑4 weeks | Yes |
| Hydrocortisone + Miconazole | Hydrocortisone 1 % + Miconazole 2 % | Low‑moderate | Broad (dermatophytes, Candida) | 2‑6 weeks | Often OTC (in some countries) |
| Ketoconazole 2 % | Ketoconazole 2 % | None (pure antifungal) | Very broad, good for seborrheic dermatitis | 4‑6 weeks | Prescription in many regions |
| Terbinafine 1 % | Terbinafine 1 % | None | Excellent for dermatophytes, weaker on Candida | 1‑2 weeks (often enough) | Prescription |
| Nystatin 100,000 IU/g | Nystatin | None | Specialized for Candida (yeast) infections | 2‑4 weeks | Prescription |
Pros and Cons of Each Option
- Lotrisone: Fast relief of inflammation + antifungal action; risk of skin thinning, systemic steroid exposure if misused.
- Hydrocortisone + Miconazole: Gentler steroid, suitable for sensitive skin; may be less effective for severe inflammation.
- Ketoconazole: Pure antifungal, good for oily/scaly areas; no steroid benefit, so itching may linger.
- Terbinafine: Short treatment duration, high cure rate for athlete’s foot; limited against Candida.
- Nystatin: Ideal for yeast infections (candida); not useful for dermatophyte‑driven rashes.
How to Choose the Right Cream
- Identify the infection type. If a doctor confirms a dermatophyte (tinea) with marked redness, Lotrisone or hydrocortisone‑miconazole are logical choices.
- Consider skin sensitivity. For thin or facial skin, avoid high‑potency steroids; opt for ketoconazole or terbinafine.
- Check treatment length. If you need a quick cure (<2 weeks), terbinafine often finishes the job faster.
- Look at availability. Some OTC combos (hydrocortisone‑miconazole) are easy to buy, while others require a prescription.
- Review side‑effect profile. Steroid‑containing creams can cause telangiectasia, striae, or adrenal suppression with over‑use.

Safety, Side Effects, and Precautions
All topical steroids share a similar risk set, scaled by potency. Betamethasone (in Lotrisone) can:
- Thin the epidermis after weeks of continuous use.
- Trigger steroid‑withdrawal rash if stopped abruptly.
- Potentially exacerbate viral skin infections (e.g., herpes simplex).
Clotrimazole is generally well‑tolerated but may cause mild burning or redness. For the alternatives, side effects are usually limited to irritation (ketoconazole) or rare allergic reactions (terbinafine).
Never apply any of these creams on large body surface areas (>10 % BSA) for longer than prescribed without medical supervision.
Real‑World Scenarios
Scenario 1 - Athlete’s foot with severe itching. A 28‑year‑old runner reports a scaly, red rash between the toes that’s painful. A prescription of Lotrisone brings rapid itch relief within a few days, and the fungal infection clears after three weeks.
Scenario 2 - Candida intertrigo in a diabetic patient. The same runner develops a moist, red, macerated rash in the groin. Because Candida responds best to Nystatin, the doctor switches to a Nystatin powder, achieving full resolution without the need for a steroid.
Scenario 3 - Mild tinea corporis on the arm. A teenager with a small, mildly inflamed ringworm patch prefers an OTC option. Hydrocortisone + Miconazole works well, offering enough anti‑inflammatory effect without the stronger steroid side‑effects.
Frequently Asked Questions
Can I use Lotrisone on my face?
Generally no. The high‑potency steroid can cause skin thinning and accelerate acne. For facial fungal infections, a pure antifungal like ketoconazole or a low‑strength steroid‑antifungal combo is safer.
How long should I keep using Lotrisone?
Most dermatologists recommend 2‑4 weeks, and never beyond 6 weeks without reassessment. If symptoms improve early, you can taper by applying every other day.
Is there an OTC alternative that works as well?
Hydrocortisone + Miconazole creams are available over the counter in many countries and provide similar relief for mild‑to‑moderate cases. They lack the potency of betamethasone, so very inflamed patches may need a prescription.
What should I do if I notice skin thinning?
Stop the steroid immediately and contact a healthcare professional. They may prescribe a steroid‑free antifungal or suggest a shorter‑acting steroid to finish the course.
Can I use Lotrisone while pregnant or breastfeeding?
Topical steroids are generally low risk, but betamethasone is a high‑potency agent. Discuss with your obstetrician; many prefer a milder steroid or pure antifungal during pregnancy.
Bottom Line
Lotrisone shines when you need fast relief from both inflammation and a fungal infection, especially on tough skin surfaces. However, its potency demands careful, time‑limited use. If your infection is mild, or if you have sensitive skin, alternatives like hydrocortisone‑miconazole, ketoconazole, terbinafine, or Nystatin may give you a safer, equally effective outcome.
Always confirm the exact cause of your rash with a clinician before starting a steroid‑antifungal combo, and follow the prescribed duration to avoid unwanted side effects.
Miracle Zona Ikhlas
Great overview-Lotrisone works fast but always respect the time limits.
naoki doe
I’ve tried Lotrisone on a stubborn athlete’s foot and felt the itch vanish within days, but I also pushed the cream for six weeks, which left the skin a bit thin. That’s why I always stress the importance of a doctor’s follow‑up. It’s easy to think “just a little longer” when the rash looks better, yet the steroid can sneak in systemically. Use the prescribed schedule or you’ll be asking for a dermatologist later.
Carolyn Cameron
The pharmacological synergy manifested by the concomitant administration of betamethasone dipropionate and clotrimazole epitomizes a paradigmatic approach to dermato‑mycotic pathologies.
From a mechanistic standpoint, the corticosteroid component attenuates the pro‑inflammatory cascade via genomic repression of NF‑κB translocation, thereby mitigating erythema and pruritus.
Concurrently, the azole moiety impedes ergosterol biosynthesis, effecting fungistatic activity against dermatophytes and Candida spp.
Such a bipartite modality confers an accelerated therapeutic index when juxtaposed with monotherapy employing either agent in isolation.
Nevertheless, the clinical literature admonishes prudence, citing cutaneous atrophy and hypothalamic‑pituitary‑adrenal axis suppression as plausible sequelae of protracted exposure.
Empirical data indicate a median duration of efficacious use spanning two to four weeks, beyond which the risk‑benefit ratio deteriorates precipitously.
In comparative trials, hydrocortisone‑miconazole formulations demonstrate comparable antifungal spectra whilst possessing markedly attenuated glucocorticoid potency.
Ketoconazole, devoid of steroidal action, excels in seborrheic contexts but may falter in ameliorating severe inflammatory discomfort.
Terbinafine’s abbreviated treatment course, typically one to two weeks, renders it a preferred option for uncomplicated tinea pedis, albeit its fungicidal activity against Candida remains suboptimal.
Nystatin, confined to anti‑Candida activity, offers a sterility‑preserving alternative when yeast predominates.
The stratification of therapeutic choice ought to be predicated upon precise mycological identification, anatomical site, and patient‑specific cutaneous tolerance.
For instance, intertriginous regions with compromised barrier function merit avoidance of high‑potency steroids to preclude maceration.
Pregnant patients, given the fetal implications of systemic corticosteroid absorption, are counseled towards low‑potency or steroid‑free regimens.
From an economic perspective, over‑the‑counter preparations such as hydrocortisone‑miconazole may alleviate financial burdens without sacrificing efficacy in mild presentations.
Adherence to a physician‑guided tapering protocol further mitigates rebound inflammation, a phenomenon occasionally observed upon abrupt cessation of potent topical steroids.
In summation, Lotrisone constitutes a valuable armamentarium for acute, inflamed fungal dermatoses, provided its deployment adheres strictly to evidenced‑based temporal constraints.
sarah basarya
Wow, that was a masterclass in jargon‑fest! If I wanted a bedtime story, I’d read a chemistry textbook, not a Reddit comment. Bottom line: Lotrisone is powerful, but you’ve got to respect it or end up with skin so thin you could see the bones. Keep it short, keep it safe.
Samantha Taylor
Ah, the classic “it works great” narrative, punctuated by a subtle reminder that steroids are not a free pass to neglect dermatological monitoring. One might argue that the allure of rapid itch relief blinds many to the insidious potential for iatrogenic atrophy. Thus, the prudent clinician will always couple prescription with a clear cessation timeline.
Joe Langner
Yea, I get the vibe-stay safe but still enjoy the quick fix. Theres a fine line betwen comfort and overdo, and I think we can learn to trust our bodies while still listening to doc advice. Keep it simple, and don’t stress too much!
Ben Dover
From a quantitative risk assessment perspective, the incidence of corticoid‑induced skin atrophy in Lotrisone users approximates 3‑5% when treatment exceeds the recommended four‑week threshold. This metric underscores the necessity of integrating pharmacovigilance protocols in outpatient management.
Katherine Brown
I appreciate the statistical framing you provided; it adds a necessary layer of objectivity to the discourse. While the numbers are indeed sobering, fostering open communication between practitioner and patient can mitigate undue apprehension and promote adherence to optimal treatment durations.
Tony Stolfa
Enough of the polite talk-if you’re not willing to follow the dosing schedule, you’re just digging your own skin holes. Either stick to the plan or quit the cream, but don’t whine about side effects you invited.



Write a comment