
Salmonellosis Risk Assessment Tool
Pregnancy Food Safety Assessment
Answer these questions to assess your Salmonella risk during pregnancy.
Risk Assessment Results
Remember: This assessment is for informational purposes only. Always consult your healthcare provider about food safety during pregnancy.
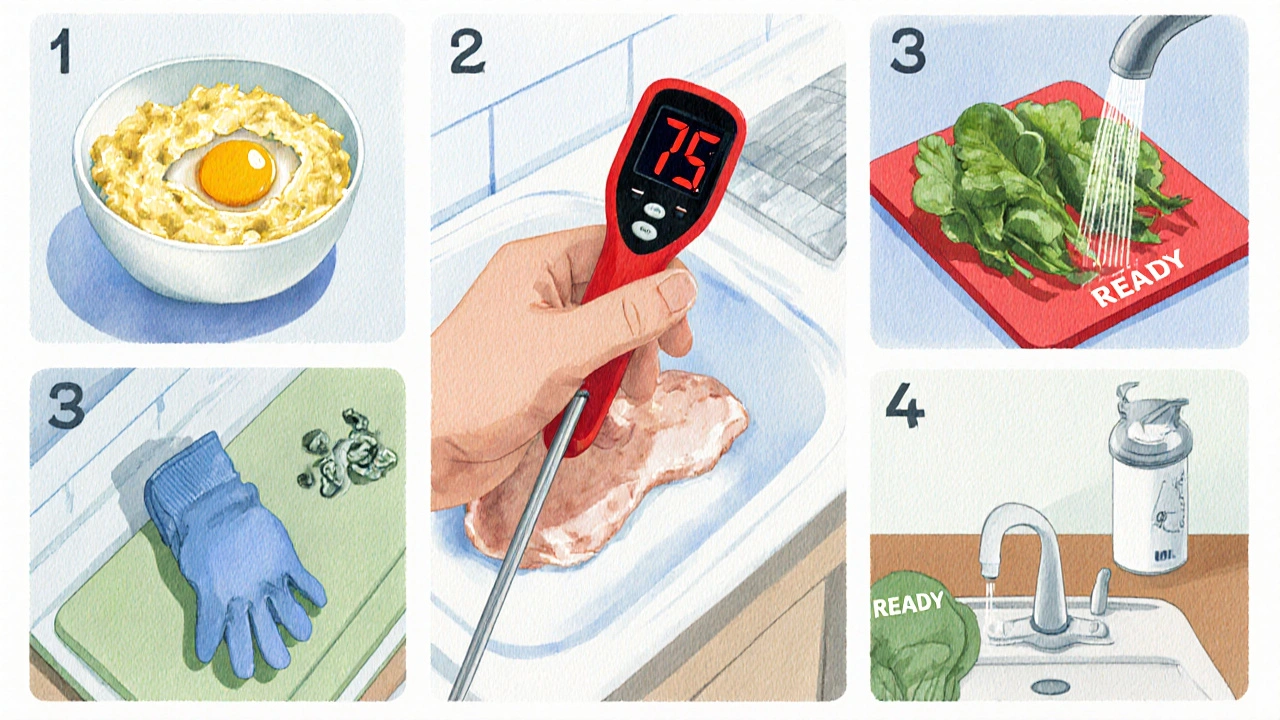
Key Recommendations
- Cook eggs until yolks are firm
- Use a food thermometer for poultry (75°C)
- Wash produce thoroughly before eating
- Avoid unpasteurized dairy products
- Refrigerate leftovers within 2 hours
When it comes to Salmonellosis is a bacterial infection caused by Salmonella species that typically triggers gastrointestinal symptoms, pregnant women need extra caution.
Key Takeaways
- Salmonellosis can cause severe dehydration and may increase miscarriage risk, especially in the first trimester.
- Typical sources include undercooked eggs, raw poultry, and contaminated produce.
- Pregnant bodies are less able to fight off infection because of hormonal changes that slow gut motility.
- Prevention hinges on strict food‑handling practices and avoiding high‑risk foods.
- If symptoms appear, seek medical care promptly; early treatment reduces complications.
What Is Salmonellosis?
Salmonellosis is a form of food poisoning caused by the Gram‑negative bacteria Salmonella. There are over 2,500 serotypes, but the most common culprits in human illness are Salmonella Enteritidis and Salmonella Typhimurium. In the United States, the CDC estimates about 1.35 million cases annually, resulting in roughly 400 deaths. In Australia, the national surveillance system records around 5,000 confirmed infections each year, with a noticeable spike during the holiday season when raw egg dishes are popular.
Why Pregnancy Changes the Risk Landscape
Pregnancy is a unique physiological state in which the immune system is deliberately modulated to tolerate the developing fetus. Two key changes increase susceptibility to Salmonella:
- Reduced gastric acidity: Hormonal shifts lower stomach acid, allowing more bacteria to survive the passage to the intestines.
- Slowed intestinal motility: Progesterone relaxes smooth muscle, extending the time bacteria can interact with the gut lining.
These factors mean that an infection that might be mild for a non‑pregnant adult can become more severe, potentially leading to dehydration, bloodstream invasion (bacteremia), or transplacental transmission.
Typical Sources & How to Spot Them
The most common vehicles for Salmonella in the Australian diet are:
- Undercooked or raw eggs (including homemade mayonnaise, hollandaise, and desserts like pavlova).
- Raw poultry or poultry products that have not reached an internal temperature of 75°C.
- Unpasteurized milk and soft cheeses made from raw milk.
- Contaminated fresh produce, especially leafy greens washed with untreated water.
- Reptile or amphibian contact - handling turtles, lizards, or their habitats can transfer Salmonella to hands.
Because the bacteria can survive in dry environments for weeks, even leftover salads or pre‑packaged meals can become risky if stored improperly.
Symptoms to Watch For
Salmonellosis usually appears 6‑72hours after exposure. The classic triad includes:
- Diarrhea (often watery, sometimes with blood)
- Abdominal cramps
- Fever (usually between 38‑40°C)
Pregnant women may also notice:
- Persistent nausea or vomiting beyond typical morning sickness
- Signs of dehydration - dry mouth, reduced urine output, dizziness
- Unexplained fatigue or rapid heart rate
If any of these symptoms last longer than 48hours, or if you develop a high fever (> 39°C), contact your health provider.
Prevention: Food Safety Guidelines
Adhering to a strict food safety plan can cut your risk dramatically. Follow these practical steps:
- Cook eggs thoroughly: Scrambled, fried, or boiled - make sure the yolk is firm.
- Heat poultry to 75°C: Use a meat thermometer; color alone isn’t reliable.
- Separate raw and ready‑to‑eat foods: Use separate cutting boards and utensils.
- Wash produce under running water: Even if you plan to peel, a quick rinse removes surface bacteria.
- Avoid unpasteurized dairy: Choose products with the “pasteurised” label.
- Practice hand hygiene: Wash hands with soap for at least 20seconds after handling raw foods, pets, or after using the bathroom.
- Store leftovers promptly: Refrigerate within two hours and reheat to steaming hot before eating.
These habits are simple but powerful. A 2023 Australian cohort study found that pregnant women who strictly followed the above guidelines had a 70% lower incidence of Salmonella infection compared with those who didn’t.
Treatment Options: What to Expect
If you’re diagnosed with salmonellosis, most cases resolve with supportive care-fluids, rest, and a bland diet. However, pregnancy can push you into the higher‑risk category where doctors may prescribe antibiotics to prevent spread.
- First‑line antibiotics: Ampicillin or ceftriaxone are commonly used because they’re safe for the fetus.
- Hospitalization: Required for severe dehydration, high fever, or evidence of bacteremia. Intravenous fluids and electrolyte monitoring are standard.
- Monitoring fetal health: Ultrasound checks may be scheduled to ensure normal growth and heart rate.
Never self‑medicate. Some antibiotics (e.g., fluoroquinolones) are contraindicated in pregnancy and could harm the baby.
When to Call a Health Professional
Prompt medical attention can prevent serious outcomes. Reach out if you experience any of the following:
- Fever lasting more than 24hours.
- Signs of dehydration - dizziness, dry skin, scant urine.
- Blood in stool or severe abdominal pain.
- Persistent vomiting that prevents you from keeping fluids down.
- Any concern about fetal movement after the second trimester.
Most Australian hospitals have a dedicated prenatal care line; they can triage you and arrange a same‑day appointment.

Salmonellosis vs. Listeriosis: A Quick Comparison for Expectant Mothers
| Aspect | Salmonellosis | Listeriosis |
|---|---|---|
| Typical source | Undercooked eggs, raw poultry, contaminated produce | Unpasteurised dairy, soft cheeses, processed meats |
| Incubation period | 6‑72hours | 1‑4weeks (can be longer) |
| Common symptoms | Diarrhea, abdominal cramps, fever | Fever, chills, flu‑like feeling, sometimes GI symptoms |
| Risk to fetus | Miscarriage (mainly first trimester), preterm labor | Stillbirth, severe neonatal infection |
| Treatment | Supportive care; safe antibiotics if severe | IV ampicillin or penicillin promptly |
Both infections demand vigilance, but Listeriosis carries a higher mortality rate for newborns, so the threshold for treatment is lower.
Common Myths Debunked
- Myth: “If I’m pregnant, I can’t eat any eggs.”
Fact: Cooked eggs are perfectly safe; the risk lies in raw or partially‑cooked eggs. - Myth: “Antibiotics cure all food poisoning.”
Fact: Many cases are viral; unnecessary antibiotics can cause resistance and harm fetal microbiome. - Myth: “If I feel fine, the infection isn’t serious.”
Fact: Silent dehydration can develop fast; pregnant bodies deplete fluids quicker.
Quick Checklist for Expectant Moms
- ✅ Verify egg dishes are fully cooked.
- ✅ Use a food thermometer for poultry.
- ✅ Wash hands after handling raw foods or pets.
- ✅ Keep perishable foods refrigerated (<4°C).
- ✅ Stay hydrated; sip oral rehydration solutions if you have diarrhea.
- ✅ Contact your prenatal care provider within 24hours of any fever.
Frequently Asked Questions
Can I eat sushi while pregnant?
Most raw fish can carry parasites or bacteria, including Salmonella. Choose cooked options like tempura or smoked fish that has been heated to 63°C.
Is it safe to take over‑the‑counter antidiarrheal meds?
Generally not. Medications like loperamide can slow gut motility, which might keep the bacteria longer in the intestines. Hydration and medical advice are preferred.
How long does Salmonellosis last during pregnancy?
Mild cases resolve in 4‑7days with proper fluid intake. Severe cases requiring antibiotics may take 10‑14days for full recovery.
Can I breast‑feed if I’ve had salmonellosis?
Yes, once you’re fever‑free for 24hours and no longer symptomatic. Breast milk itself isn’t a transmission route.
What’s the difference between food poisoning and a stomach flu?
Food poisoning is caused by ingesting bacteria, viruses, or toxins, while stomach flu (viral gastroenteritis) usually spreads person‑to‑person. Both cause similar symptoms, but a recent high‑risk food exposure points to food poisoning.
Matt Stone
Stop ignoring the raw egg warning, it's a legit risk.
Joy Luca
The pathophysiological cascade triggered by Salmonella enterica serovar Typhimurium involves epithelial invasion, macrophage activation, and cytokine release that can amplify systemic inflammatory burden especially in gestational immunomodulation contexts; leveraging molecular diagnostics such as PCR panels can stratify risk exposure; incorporating food safety protocols aligns with evidence‑based obstetric guidelines; consideration of thermostatic validation using calibrated probes ensures poultry reaches the 75 °C threshold; adopting a multi‑modal approach integrating nutritional counseling and microbiological surveillance optimizes maternal‑fetal outcomes; thus the recommendation matrix should reflect both quantitative risk scoring and qualitative behavioral adherence.
Jessica Martins
The article outlines clear steps, but remember that personal habits matter more than generic advice; always wash hands after touching raw meat, and keep a thermometer handy; storing leftovers promptly can prevent bacterial growth; these practices are simple yet effective.
Doug Farley
Oh great, another checklist so we can all pretend we’re chefs and not pregnant women worrying about a spoonful of salmonella. If you wanted drama, read the novel instead of a health article.
Jeremy Olson
While humor has its place, the seriousness of food‑borne illness during pregnancy cannot be overstated. Healthcare providers recommend strict adherence to the guidelines presented, especially regarding temperature control and avoidance of unpasteurized products. Following these measures reduces the likelihood of maternal infection and protects fetal development.
Ada Lusardi
💧💙 staying hydrated and keeping those leftovers chilled is 🔑 for us moms‑to‑be! 😅
Pam Mickelson
Great rundown! Just a heads‑up: when you’re scrambling eggs, make sure the whites are firm and the yolk isn’t runny-that’s the sweet spot for safety. Keep the vibes positive and the kitchen clean!
Joe V
Honestly, the risk isn’t rocket science-just basic hygiene and cooking temps. If you can handle a microwave, you can handle a thermometer.
Scott Davis
Agreed. A quick check with a probe is all it takes.
Calvin Smith
Wow, who knew cooking eggs could be such a high‑stakes thriller? Next thing you know, we’ll need a PhD to make a sandwich.
Brenda Hampton
Curious about the exact temperature range where Salmonella dies off-does a quick boil guarantee safety, or do we still need that precise 75 °C mark for poultry?
Lara A.
Listen, the government doesn’t want you to know that most of these “rules” are just to keep you buying their fancy thermometers!!! It’s all a ploy to control our food choices…
Ashishkumar Jain
Bro, i think ur overthinking it. Just cook the meat good, wash the fruit, and u’ll be fine. No need for all that extra drama, y’know?
Gayatri Potdar
They’re hiding the truth about dairy! Unpasteurised cheese is a covert weapon, folks-don’t be fooled by the “health” press releases. Only the brave know the real story.
Marcella Kennedy
First of all, congratulations to every expectant mother reading this; navigating food safety while dealing with hormonal changes and a growing belly is no small feat. It’s essential to recognize that Salmonella isn’t just a fleeting inconvenience-it can cascade into dehydration, severe gastrointestinal distress, and in rare cases, impact fetal development through maternal fever and systemic inflammation. That’s why the checklist emphasizes cooking eggs until the yolk is firm; the proteins in the egg white denature at lower temperatures, but the yolk can still harbor viable bacteria if it remains runny. Using a calibrated food thermometer for poultry is another cornerstone: the target of 75 °C (or 165 °F) isn’t arbitrary, it’s the scientifically validated point where Salmonella spp. are reliably killed. Don’t rely on color alone; a pink interior can be deceptive, especially in younger birds.
When it comes to produce, a thorough rinse under running water removes surface contaminants, but remember that some pathogens can embed in crevices; a vinegar solution can offer an extra layer of protection without compromising the nutrients. As for dairy, the “pasteurised” label is your friend-unpasteurised milks and cheeses increase the risk of not just Salmonella but also Listeria, which is even more dangerous during pregnancy. Hand hygiene is another non‑negotiable: twenty seconds of soap after handling raw foods, pets, or using the restroom dramatically reduces cross‑contamination.
Storing leftovers within two hours is critical because the bacterial growth curve accelerates rapidly in the so‑called “danger zone” of 4 °C to 60 °C. Refrigerate promptly, and when reheating, ensure the food reaches steaming hot temperatures throughout; a quick microwave blast can miss cold spots, so stir and check. It’s also wise to label leftovers with dates to avoid accidental consumption of food that’s been stored too long.
If symptoms do appear-persistent fever, blood in stool, severe abdominal pain, or signs of dehydration-seek medical attention without delay. Pregnant women have a lower threshold for complications, and early intervention with appropriate antibiotics (such as ampicillin or ceftriaxone, which are considered safe for the fetus) can prevent progression to more serious illness. Finally, keep open communication with your prenatal care provider; they can tailor advice to your personal health history and local outbreak data. Stay vigilant, stay informed, and most importantly, stay healthy for both you and your little one.
Jamie Hogan
One must appreciate the epistemic rigor underpinning the recommended culinary thresholds; the thermodynamic parameters delineated are not mere suggestions but empirically substantiated imperatives for obstetric safety.
Ram Dwivedi
Hey everyone 😊! Quick tip: Keep a small digital thermometer in your kitchen drawer-it’s cheap and can save you a lot of worry later. Also, if you ever feel unsure about leftovers, just give them a good reheating once more. Stay safe! 🌟
pooja shukla
Listen, these western food‑safety hacks are nothing compared to what we practice back home; we’ve been handling raw poultry for generations without the need for overpriced gadgets. Trust your instincts and traditional methods-they’re far more reliable than any imported thermometer.




Write a comment