What Psoriasis Really Is - And Why Treatment Has Changed
Psoriasis isn’t just dry, flaky skin. It’s an immune system mistake. Your body attacks its own skin cells, making them grow too fast and pile up into thick, red patches. This isn’t contagious. It’s not caused by poor hygiene. It’s genetic, inflammatory, and often tied to other health problems like heart disease, diabetes, and joint pain. Around 125 million people worldwide live with it. In Australia, about 2-3% of the population has some form - and most of them have plaque psoriasis.
For decades, doctors treated psoriasis like a surface problem. Steroid creams, coal tar, light therapy - all aimed at calming the skin. But now we know: the real issue is inside. It’s the immune system, firing off signals like TNF-alpha, IL-17, and IL-23. These molecules tell skin cells to multiply like crazy. Treatments today don’t just cover up the rash - they shut down the message.
Plaque Psoriasis: The Most Common Form, The Hardest to Ignore
Eight out of ten people with psoriasis have plaque type. That’s the thick, silvery scales on elbows, knees, scalp, and lower back. It’s visible. It itches. It burns. It hurts to wear clothes. And it doesn’t always respond to over-the-counter lotions.
For mild cases - under 5% of body surface - topical treatments still work. Corticosteroids, especially class III or IV, are the go-to. But they can’t be used long-term on the face or folds. That’s where calcipotriol (a vitamin D analog) comes in. Used with a steroid, it clears up to 40% of plaques in eight weeks. Newer options like tapinarof cream (1%) work differently - they calm inflammation without steroids. In trials, about one-third of users saw 75% improvement by week 12.
But if you’ve got plaques on your scalp, nails, or genitals? That’s a different game. For scalp psoriasis, a foam with calcipotriol and betamethasone works in 89% of cases. For nail psoriasis, a shot of triamcinolone directly into the nail bed can reduce pitting by 75% in 12 weeks. These aren’t guesses - they’re proven techniques used by dermatologists every day.
Guttate Psoriasis: When Infection Triggers a Rain of Spots
Guttate psoriasis looks nothing like plaque. It’s small, teardrop-shaped red dots - often all over the torso, arms, and legs. It usually shows up after a strep throat infection, especially in kids and young adults. One study found that 80% of guttate cases followed a strep bug within two weeks.
Here’s the good news: guttate psoriasis often clears on its own in weeks or months. But if it doesn’t, or if it turns into plaque, you need to act. Mild cases respond to topical steroids or light therapy. For stubborn cases, doctors may use methotrexate or cyclosporine - but only short-term. Why? Because these drugs suppress the immune system. You don’t want to keep them going if the psoriasis might fade.
Biologics? Usually not the first choice for guttate. But if it keeps coming back, or if you’re developing joint pain, switching to an IL-23 inhibitor like guselkumab can stop the cycle. One patient I spoke to - a 22-year-old student - had three guttate flares in two years after strep. After starting guselkumab, she hasn’t had a flare in 18 months.
Systemic Treatments: When Topicals Aren’t Enough
If psoriasis covers more than 5-10% of your skin, or if it’s affecting your quality of life - sleep, work, relationships - then it’s time to think beyond creams. That’s where systemic treatments come in. These work inside your body. They’re not just stronger. They’re smarter.
Oral meds like methotrexate, acitretin, and apremilast have been around for years. Methotrexate clears 50-60% of plaques in 16 weeks. But it needs blood tests every few weeks. Apremilast (Otezla) is easier - one pill twice a day. But it’s slower. Only 33% hit 75% clearance. And it can cause nausea and diarrhea.
Then there’s deucravacitinib. It’s new. It’s oral. It blocks a specific enzyme (TYK2) that drives psoriasis inflammation. In trials, nearly 60% of users saw 75% skin clearance at 16 weeks. No injections. No blood draws. Just a daily pill. It’s becoming a favorite for patients who hate needles but need real results.
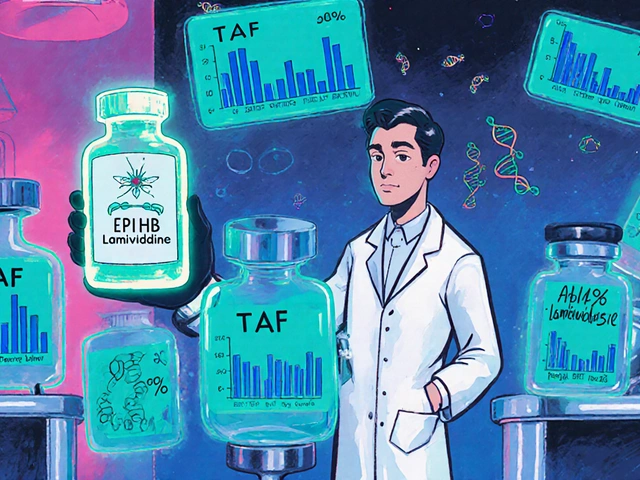
Biologics: The Game Changers
Biologics are the most powerful tools we have. They’re made from living cells, designed to target one specific part of the immune system. There are three main types: TNF blockers, IL-17 inhibitors, and IL-23 inhibitors.
TNF inhibitors like adalimumab (Humira) were the first. They work - about 78% get 75% clearance. But they’re old. They’re expensive. And they can increase the risk of infections.
IL-17 inhibitors like secukinumab (Cosentyx) are faster. You see results in two weeks. About 79% hit 90% clearance. But if you have Crohn’s disease or IBD, these aren’t safe. They can make it worse.
IL-23 inhibitors - guselkumab (Tremfya), risankizumab (Skyrizi), tildrakizumab (Ilumya) - are now the gold standard. Why? Because they’re more effective, safer for the gut, and you only need to inject them every 8 to 12 weeks. Guselkumab clears 84% of plaques to 90% or better. In real-world use, 78% of patients stick with it after a year. That’s higher than any other biologic.
And here’s something most people don’t know: IL-23 inhibitors work better on scalp and nail psoriasis than older drugs. Guselkumab cleared scalp psoriasis in 74% of patients - compared to 62% with ustekinumab. For people with stubborn nail pits or thick scalp scales, this is life-changing.
Cost, Access, and What You Can Actually Afford
Let’s be real. Biologics cost a lot. Guselkumab runs about $34,200 a year. Secukinumab is $32,800. Even the oral drugs like apremilast hit $7,200. That’s not something most people can pay out of pocket.
But here’s the catch: 85% of insured patients pay $0 to $150 a month thanks to manufacturer assistance programs. If you’re on Medicare or private insurance, you likely qualify. You just have to ask. Dermatologists now use electronic prior authorization systems. Approval time dropped from two weeks to under six days in 2025.
Some patients still struggle. If you’re underinsured or on Medicaid, ask about patient assistance foundations. The National Psoriasis Foundation helps over 10,000 Australians yearly. They’ll help you fill out forms, find free samples, and connect with nurses who teach you how to inject yourself at home.
What’s Coming Next - And What You Should Watch For
The next wave of psoriasis treatment isn’t just about better drugs. It’s about better delivery. Oral peptides - pills that act like biologics - are in phase 3 trials. Early results show 82% skin clearance, with no injections. One drug, vunakizumab, cleared 86% of plaques in 16 weeks. It could be approved by 2026.
Another exciting area: stopping treatment. The GUIDE trial is testing whether patients who get 100% clearance on guselkumab can stop altogether - and stay clear. Early data shows some do. That’s huge. It means psoriasis might not be lifelong for everyone.
For now, if you’ve tried topicals and still have plaques, don’t wait. Talk to your dermatologist about biologics. Don’t assume you’re not a candidate. The new guidelines say: if your Psoriasis Area and Severity Index (PASI) is over 10, or your DLQI (quality of life score) is over 10, you’re eligible. That’s not severe. That’s moderate. And it’s enough to justify treatment.
Real Patient Stories - What Works, What Doesn’t
One Reddit user, u/PsoriasisWarrior, tried methotrexate and Humira. Neither worked. He switched to guselkumab. Three months later, 95% of his plaques were gone. He gets injections every 12 weeks. Cost? $500 a month with insurance. He says it’s worth it.
Another, on Drugs.com, tried secukinumab for a job interview. Took four months to work. She needed faster relief. She switched to risankizumab. Saw improvement in three weeks.
But not everyone wins. Some patients don’t respond to IL-17 blockers because their psoriasis is driven by a different immune signal - type I interferon. That’s why doctors now use gene testing to classify psoriasis into subtypes. If your first biologic fails, don’t just try another. Ask: is this the right target for my type?
What to Do If You’re Struggling
If your skin isn’t improving:
- Check your application technique. Topical steroids need to be rubbed in gently, not smeared. Use the fingertip unit method - one unit covers two adult palms.
- Don’t stop creams just because you feel better. Keep using them to prevent flare-ups.
- Use a humidifier in winter. Dry air makes psoriasis worse.
- Track your triggers. Stress, alcohol, smoking, and infections can all spark flares.
- Ask about telehealth. Many clinics now offer virtual check-ins for biologic follow-ups.
If you’re scared of needles, ask about oral options. Deucravacitinib and apremilast aren’t perfect - but they’re real alternatives. And if cost is stopping you, reach out to patient support programs. You’re not alone. There are resources. You just have to ask.
robert cardy solano
I’ve had plaque psoriasis since I was 19. Tried everything. Steroids made my skin thin out like tissue paper. Then I got on guselkumab. 12 weeks in, my elbows look normal. No more shame wearing short sleeves. Honestly? Life-changing. I didn’t think I’d ever feel comfortable at the pool again.
Brianna Groleau
I’m from India and my cousin here has guttate psoriasis after a bad strep throat. We didn’t even know it was psoriasis at first - thought it was an allergic reaction. Took us months to get a proper diagnosis. The fact that it often clears on its own gave us hope, but when it came back, we were scared. Now she’s on a low-dose biologic and her skin’s been clear for 8 months. So glad these treatments exist.
Nick Naylor
IL-23 inhibitors? Yes. But let’s not ignore the fact that Big Pharma is pushing these like candy. Guselkumab costs $34K a year? And you’re telling me the average person can afford it? Meanwhile, the FDA approves another $10K/month pill while Medicare denies coverage for half the patients. This isn’t medicine - it’s a profit model disguised as science.
Pawan Jamwal
In India, we don’t have access to any of this. My uncle tried coal tar and neem oil. He got some relief. But no biologics. No guselkumab. No oral TYK2 inhibitors. We’re lucky if we get a dermatologist who doesn’t just say ‘use moisturizer.’ This is a first-world problem. And you’re all acting like it’s a miracle. It’s not. It’s privilege.
Lemmy Coco
i just wanted to say thank you for writing this. i’ve been avoiding the dr for years cause i thought it was just ‘dry skin’ and i’d feel dumb asking. but after reading this i made an appt and asked about deucravacitinib. they said i’m a candidate. i’m nervous about taking a pill but… i’m so tired of hiding my legs. thank you.
serge jane
There’s something deeper here than just immune pathways and cytokines. Psoriasis isn’t just a disease - it’s a mirror. It reflects stress, isolation, trauma, the weight of living in a world that doesn’t see you unless you’re perfect. I used to wear long sleeves in summer. I used to avoid mirrors. I used to cry in the shower. The drugs helped my skin. But what really healed me was learning to stop apologizing for existing. The science is incredible. But the humanity? That’s the real breakthrough.
Cinkoon Marketing
My dermatologist told me to try tapinarof. I did. First week: it burned like hell. Second week: my skin felt like sandpaper. Third week: the redness started fading. By week 10, my knee plaques were gone. No steroids. No injections. Just a cream that works differently. It’s not magic. But it’s real. And I’m not going back.
Sarah Swiatek
Let’s be real - most of us don’t care about TNF-alpha vs IL-23. We care about whether we can wear a tank top without feeling like a monster. The science is cool. But the only thing that matters is: does it work? And does it let me live? Guselkumab worked for me. My husband cried when he saw my back for the first time in 7 years. That’s not a statistic. That’s a life.
rob lafata
You people are so naive. Biologics don’t cure psoriasis. They suppress your immune system so your body forgets to attack itself. And what happens when you stop? It comes back harder. And what about the cancer risk? The TB reactivation? The liver damage? You’re trading one nightmare for another and calling it progress. Wake up. This isn’t treatment. It’s chemical surrender.
Rusty Thomas
I tried everything. Even the weird stuff - apple cider vinegar, turmeric paste, cryotherapy. Nothing worked. Then I got on risankizumab. Two weeks later, my scalp looked like it did before I was 12. I haven’t had a flare in 14 months. I’m not saying it’s perfect. But it’s the first time I’ve felt like me again. And yes, I cry when I see my reflection now. So what?
Matthew McCraney
I’ve been following this since 2020. I’ve seen the same people post the same stories. ‘My skin is clear!’ ‘I’m cured!’ But then they disappear. And the next year, they’re back. Because it’s not cured. It’s suppressed. And the pharmaceutical companies know it. They’re selling hope like it’s a subscription. And we’re all just clicking ‘subscribe’ because we’re desperate.
Bill Camp
One sentence: I got my first biologic injection yesterday. My hands were shaking. I cried. I didn’t know if I was scared or hopeful. But when I looked down at my arms today - no plaques. Just skin. Real skin. I’m not okay. I’m better.



Write a comment